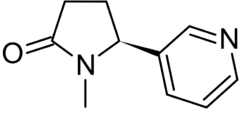
Chemistry:Cotinine
 | |
| Clinical data | |
|---|---|
| Routes of administration | Oral, Smoked, Insufflation |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Elimination half-life | 20 hours |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C10H12N2O |
| Molar mass | 176.219 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Cotinine is an alkaloid found in tobacco and is also the predominant metabolite of nicotine,[1][2] typically used as a biomarker for exposure to tobacco smoke. Cotinine is currently being studied as a treatment for depression, post-traumatic stress disorder (PTSD), schizophrenia, Alzheimer's disease and Parkinson's disease. Cotinine was developed as an antidepressant as a fumaric acid salt, cotinine fumarate, to be sold under the brand name Scotine, but it was never marketed.[1]
Similarly to nicotine, cotinine binds to, activates, and desensitizes neuronal nicotinic acetylcholine receptors, though at much lower potency in comparison.[2][3][4][5] It has demonstrated nootropic and antipsychotic-like effects in animal models.[6][7] Cotinine treatment has also been shown to reduce depression, anxiety, and fear-related behavior as well as memory impairment in animal models of depression, post-traumatic stress disorder, and Alzheimer's disease.[8] Nonetheless, treatment with cotinine in humans was reported to have no significant physiologic, subjective, or performance effects in one study,[9] though others suggest that this may not be the case.[10]
Because cotinine is the main metabolite to nicotine and has been shown to be pharmacologically active, it has been suggested that some of nicotine's effects in the nervous system may be mediated by cotinine and/or complex interactions with nicotine itself.[8][11]
Pharmacology
A few studies indicate that the affinity for cotinine to the nicotinic acetylcholine receptors (nAChRs) is about 100 times lower than nicotine's.[10] Some work suggests that cotinine may be a positive allosteric modulator of α7 nAChRs.[12][10] If this is true, cotinine would facilitate endogenous neurotransmission without directly stimulating nAChRs.
Pharmacokinetics
Cotinine has an in vivo half-life of approximately 20 hours, and is typically detectable for several days (up to one week) after the use of tobacco. The level of cotinine in the blood, saliva, and urine is proportionate to the amount of exposure to tobacco smoke, so it is a valuable indicator of tobacco smoke exposure, including secondary (passive) smoke.[13] People who smoke menthol cigarettes may retain cotinine in the blood for a longer period because menthol can compete with enzymatic metabolism of cotinine.[14] African American smokers generally have higher plasma cotinine levels than Caucasian smokers.[15] Males generally have higher plasma cotinine levels than females.[16] These systematic differences in cotinine levels were attributed to variation in CYP2A6 activity.[17] At steady state, plasma cotinine levels are determined by the amount of cotinine formation and the rate of cotinine removal, which are both mediated by the enzyme CYP2A6.[17] Since CYP2A6 activity differs by sex (estrogen induces CYP2A6) and genetic variation, cotinine accumulates in individuals with slower CYP2A6 activity, resulting in substantial differences in cotinine levels for a given tobacco exposure.[17]
Detection in body fluids
Drug tests can detect cotinine in the blood, urine, or saliva. Salivary cotinine concentrations are highly correlated to blood cotinine concentrations, and can detect cotinine in a low range, making it the preferable option for a less invasive method of tobacco exposure testing. Urine cotinine concentrations average four to six times higher than those in blood or saliva, making urine a more sensitive matrix to detect low-concentration exposure.[18]
Cotinine levels <10 ng/mL are considered to be consistent with no active smoking. Values of 10 ng/mL to 100 ng/mL are associated with light smoking or moderate passive exposure, and levels above 300 ng/mL are seen in heavy smokers — more than 20 cigarettes a day. In urine, values between 11 ng/mL and 30 ng/mL may be associated with light smoking or passive exposure, and levels in active smokers typically reach 500 ng/mL or more. In saliva, values between 1 ng/mL and 30 ng/mL may be associated with light smoking or passive exposure, and levels in active smokers typically reach 100 ng/mL or more.[19] Cotinine assays provide an objective quantitative measure that is more reliable than smoking histories or counting the number of cigarettes smoked per day. Cotinine also permits the measurement of exposure to second-hand smoke (passive smoking).
However, tobacco users attempting to quit with the help of nicotine replacement therapies (i.e., gum, lozenge, patch, inhaler, and nasal spray) will also test positive for cotinine, since all common NRT therapies contain nicotine that is metabolized in the same way. Therefore, the presence of cotinine is not a conclusive indication of tobacco use.[20] Cotinine levels can be used in research to explore the question of the amount of nicotine delivered to the user of e-cigarettes, where laboratory smoking machines have many problems replicating real-life conditions.[21]
Serum cotinine concentration has been used for decades in US population surveys of the Centers for Disease Control and Prevention to monitor tobacco use, to monitor levels and trends in exposure to environmental tobacco smoke, and to study the relationship between tobacco smoke and chronic health conditions.[22] An estimated one in four nonsmokers (approximately 58 million persons) were exposed to secondhand smoke during 2013-2014. Nearly 40% of children aged 3–11 years were exposed as were 50% of non-Hispanic blacks.
References
- ↑ 1.0 1.1 Dictionary of Pharmacological Agents. Boca Raton: Chapman & Hall/CRC. 1996. ISBN 978-0-412-46630-4. https://books.google.com/books?id=DeX7jgInYFMC&q=scotine%20cotinine&pg=PA522.
- ↑ 2.0 2.1 "(S)-(-)-Cotinine, the major brain metabolite of nicotine, stimulates nicotinic receptors to evoke [3Hdopamine release from rat striatal slices in a calcium-dependent manner"]. The Journal of Pharmacology and Experimental Therapeutics 288 (3): 905–911. March 1999. PMID 10027825. http://jpet.aspetjournals.org/cgi/pmidlookup?view=long&pmid=10027825.
- ↑ "Nicotinic receptor binding of [3H]cytisine, [3H]nicotine and [3H]methylcarbamylcholine in rat brain". European Journal of Pharmacology 253 (3): 261–267. March 1994. doi:10.1016/0014-2999(94)90200-3. PMID 8200419.
- ↑ "Activation and inhibition of the human alpha7 nicotinic acetylcholine receptor by agonists". Neuropharmacology 37 (9): 1095–1102. September 1998. doi:10.1016/S0028-3908(98)00110-5. PMID 9833639.
- ↑ "Disconnection between activation and desensitization of autonomic nicotinic receptors by nicotine and cotinine". Neuroscience Letters 413 (1): 68–71. February 2007. doi:10.1016/j.neulet.2006.11.028. PMID 17157984.
- ↑ "A reversible model of the cognitive impairment associated with schizophrenia in monkeys: potential therapeutic effects of two nicotinic acetylcholine receptor agonists". Biochemical Pharmacology 78 (7): 852–862. October 2009. doi:10.1016/j.bcp.2009.06.102. PMID 19577545.
- ↑ "Desensitization of nicotinic acetylcholine receptors as a strategy for drug development". The Journal of Pharmacology and Experimental Therapeutics 328 (2): 364–370. February 2009. doi:10.1124/jpet.108.145292. PMID 19023041.
- ↑ 8.0 8.1 "New Insights into the Mechanisms of Action of Cotinine and its Distinctive Effects from Nicotine". Neurochemical Research 40 (10): 2032–2046. October 2015. doi:10.1007/s11064-014-1359-2. PMID 24970109.
- ↑ "Safety of cotinine in humans: physiologic, subjective, and cognitive effects". Pharmacology, Biochemistry, and Behavior 57 (4): 643–650. August 1997. doi:10.1016/s0091-3057(97)80001-9. PMID 9258989.
- ↑ 10.0 10.1 10.2 "Cotinine: Beyond that Expected, More than a Biomarker of Tobacco Consumption". Frontiers in Pharmacology 3: 173. Oct 2012. doi:10.3389/fphar.2012.00173. PMID 23087643.
- ↑ "Contribution of CNS nicotine metabolites to the neuropharmacological effects of nicotine and tobacco smoking". Biochemical Pharmacology 54 (7): 743–753. October 1997. doi:10.1016/s0006-2952(97)00117-2. PMID 9353128.
- ↑ "Potentiation of alpha7 nicotinic acetylcholine receptors via an allosteric transmembrane site". Proceedings of the National Academy of Sciences of the United States of America 105 (38): 14686–14691. September 2008. doi:10.1073/pnas.0804372105. PMID 18791069.
- ↑ "Methods for quantification of exposure to cigarette smoking and environmental tobacco smoke: focus on developmental toxicology". Therapeutic Drug Monitoring 31 (1): 14–30. February 2009. doi:10.1097/FTD.0b013e3181957a3b. PMID 19125149.
- ↑ "Signs of smoking linger longer in menthol smokers". Center for the Advancement of Health. Science Blog. December 2002. http://www.scienceblog.com/community/older/2002/G/20021531.html.
- ↑ "Racial differences in serum cotinine levels among smokers in the Coronary Artery Risk Development in (Young) Adults study". American Journal of Public Health 80 (9): 1053–1056. September 1990. doi:10.2105/ajph.80.9.1053. PMID 2382740.
- ↑ "Sex-related differences in serum cotinine concentrations in daily cigarette smokers". Nicotine & Tobacco Research 10 (8): 1293–1300. August 2008. doi:10.1080/14622200802239132. PMID 18686176.
- ↑ 17.0 17.1 17.2 "The ability of plasma cotinine to predict nicotine and carcinogen exposure is altered by differences in CYP2A6: the influence of genetics, race, and sex". Cancer Epidemiology, Biomarkers & Prevention 22 (4): 708–718. April 2013. doi:10.1158/1055-9965.EPI-12-1234-T. PMID 23371292.
- ↑ Avila-Tang, Erika et al (September 2012). "Assessing secondhand smoke using biological markers" - Nicotine and metabolites [1]. Retrieved 10 June 2013
- ↑ "Assessing smoking status in children, adolescents and adults: cotinine cut-points revisited". Addiction 103 (9): 1553–1561. September 2008. doi:10.1111/j.1360-0443.2008.02297.x. PMID 18783507. https://discovery.ucl.ac.uk/id/eprint/6751/.
- ↑ "Reasons for False Positives for Nicotine on a Blood Test". LiveStrong.com. http://www.livestrong.com/article/26557-reasons-false-positives-nicotine-blood/.
- ↑ "E-cigarettes: an evidence update. A report commissioned by Public Health England". UK: Public Health England. 2015. pp. 70–75. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/454516/Ecigarettes_an_evidence_update_A_report_commissioned_by_Public_Health_England.pdf.
- ↑ "Exposure to Secondhand Smoke Among Nonsmokers - United States, 1988-2014". MMWR. Morbidity and Mortality Weekly Report 67 (48): 1342–1346. December 2018. doi:10.15585/mmwr.mm6748a3. PMID 30521502.
 |

