Chemistry:Beta blocker
| Beta blockers | |
|---|---|
| Drug class | |
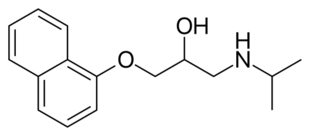 Skeletal formula of propranolol, the first clinically successful beta blocker. | |
| Class identifiers | |
| Synonyms | beta-blockers, β-blockers, beta-adrenergic blocking agents, beta antagonists, beta-adrenergic antagonists, beta-adrenoreceptor antagonists, beta adrenergic receptor antagonists, BB |
| Use | Hypertension, arrhythmia, etc. |
| ATC code | C07 |
| Biological target | beta receptors |
| Clinical data | |
| Drugs.com | Drug Classes |
| Consumer Reports | Best Buy Drugs |
| WebMD | MedicineNet RxList |
| External links | |
| MeSH | D000319 |
Beta blockers, also spelled β-blockers, are a class of medications that are predominantly used to manage abnormal heart rhythms (arrhythmia), and to protect the heart from a second heart attack after a first heart attack (secondary prevention).[1] They are also widely used to treat high blood pressure, although they are no longer the first choice for initial treatment of most patients.[2]
Beta blockers are competitive antagonists that block the receptor sites for the endogenous catecholamines epinephrine (adrenaline) and norepinephrine (noradrenaline) on adrenergic beta receptors, of the sympathetic nervous system, which mediates the fight-or-flight response.[3]:152[4] Some block activation of all types of β-adrenergic receptors and others are selective for one of the three known types of beta receptors, designated β1, β2 and β3 receptors.[3]:153 β1-adrenergic receptors are located mainly in the heart and in the kidneys.[4] β2-adrenergic receptors are located mainly in the lungs, gastrointestinal tract, liver, uterus, vascular smooth muscle, and skeletal muscle.[4] β3-adrenergic receptors are located in fat cells.[5]
Beta receptors are found on cells of the heart muscles, smooth muscles, airways, arteries, kidneys, and other tissues that are part of the sympathetic nervous system and lead to stress responses, especially when they are stimulated by epinephrine (adrenaline). Beta blockers interfere with the binding to the receptor of epinephrine and other stress hormones and weaken the effects of stress hormones.
In 1964, James Black[6] synthesized the first clinically significant beta blockers—propranolol and pronethalol; it revolutionized the medical management of angina pectoris[7] and is considered by many to be one of the most important contributions to clinical medicine and pharmacology of the 20th century.[8]
For the treatment of primary hypertension, meta-analyses of studies which mostly used atenolol have shown that although beta blockers are more effective than placebo in preventing stroke and total cardiovascular events, they are not as effective as diuretics, medications inhibiting the renin–angiotensin system (e.g., ACE inhibitors), or calcium channel blockers.[9][10][11][12]
Medical uses
Beta blockers are utilized in the treatment of various conditions related to the heart and vascular system, as well as several other medical conditions. Common heart-related conditions for which beta blockers are well-established include angina pectoris, acute coronary syndromes, hypertension, and arrhythmias such as atrial fibrillation and heart failure. They are also used in the management of other heart diseases, such as hypertrophic obstructive cardiomyopathy, mitral valve stenosis or prolapse, and dissecting aneurysm. Additionally, beta blockers find applications in vascular surgery, the treatment of anxiety states, cases of thyrotoxicosis, glaucoma, migraines, and esophageal varices.[13]
Congestive heart failure
Although beta blockers were once contraindicated in congestive heart failure, as they have the potential to worsen the condition due to their effect of decreasing cardiac contractility, studies in the late 1990s showed their efficacy at reducing morbidity and mortality.[14][15][16] Bisoprolol, carvedilol, and sustained-release metoprolol are specifically indicated as adjuncts to standard ACE inhibitor and diuretic therapy in congestive heart failure, although at doses typically much lower than those indicated for other conditions. Beta blockers are only indicated in cases of compensated, stable congestive heart failure; in cases of acute decompensated heart failure, beta blockers will cause a further decrease in ejection fraction, worsening the patient's current symptoms.[citation needed]
Beta blockers are known primarily for their reductive effect on heart rate, although this is not the only mechanism of action of importance in congestive heart failure.[17] Beta blockers, in addition to their sympatholytic β1 activity in the heart, influence the renin–angiotensin system at the kidneys. Beta blockers cause a decrease in renin secretion, which in turn reduces the heart oxygen demand by lowering the extracellular volume and increasing the oxygen-carrying capacity of the blood. Heart failure characteristically involves increased catecholamine activity on the heart, which is responsible for several deleterious effects, including increased oxygen demand, propagation of inflammatory mediators, and abnormal cardiac tissue remodeling, all of which decrease the efficiency of cardiac contraction and contribute to the low ejection fraction.[18] Beta blockers counter this inappropriately high sympathetic activity, eventually leading to an improved ejection fraction, despite an initial reduction in ejection fraction.[citation needed]
Trials have shown beta blockers reduce the absolute risk of death by 4.5% over a 13-month period. In addition to reducing the risk of mortality, the numbers of hospital visits and hospitalizations were also reduced in the trials.[19] A 2020 Cochrane review found minimal evidence to support the use of beta blockers in congestive heart failure in children, however did identify that from the data available, that they may be of benefit.[20]
Therapeutic administration of beta blockers for congestive heart failure ought to begin at very low doses (1/8 of target) with a gradual escalation of the dose. The heart of the patient must adjust to decreasing stimulation by catecholamines and find a new equilibrium at a lower adrenergic drive.[21]
Acute Myocardial Infarction
Beta blockers are indicated for the treatment of acute myocardial infarctions. During a myocardial infarction, systemic stress causes an increase in circulating catecholamines.[22][23] This results an increase in heart rate and blood pressure, therefore increasing myocardial oxygen demand.[23][22] Beta blockers competitively inhibit catecholamines acting on the β1-adrenergic receptors, thus reducing these detrimental effects and resulting in reduced myocardial oxygen consumption and demand.[22]
A 2019 Cochrane review compared beta blockers with placebo or no intervention, it found that beta blockers probably reduced the short-term risk of reinfarction and the long-term risk of all-cause mortality and cardiovascular mortality.[22] The review identified that beta blockers likely had little to no impact on short-term all-cause mortality and cardiovascular mortality.[22]
Hypertension
Beta blockers are widely used for the treatment of hypertension.[24]
A 2014 Cochrane review found that in individuals with mild-to-moderate hypertension, non-selective beta blockers led to a reduction of -10/-7mmHg (systolic/diastolic) without increased rates of adverse events.[25] At higher doses, it was found to increase the rate of adverse effects such as a reduction in heart rate, without a corresponding reduction in blood pressure.[25]
A 2017 Cochrane review on the use of beta blockers in hypertension found a modest reduction in cardiovascular disease but little to no change in mortality[26] It suggested that the effects of beta blockers are inferior to other anti-hypertensive medications.[26]
Anxiety
Officially, beta blockers are not approved for anxiolytic use by the U.S. Food and Drug Administration.[27] However, many controlled trials in the past 25 years indicate beta blockers are effective in anxiety disorders, though the mechanism of action is not known.[28] The physiological symptoms of the fight-or-flight response (pounding heart, cold/clammy hands, increased respiration, sweating, etc.) are significantly reduced, thus enabling anxious individuals to concentrate on the task at hand.[citation needed]
Musicians, public speakers, actors, and professional dancers have been known to use beta blockers to avoid performance anxiety, stage fright, and tremor during both auditions and public performances. The application to stage fright was first recognized in The Lancet in 1976, and by 1987, a survey conducted by the International Conference of Symphony Orchestra Musicians, representing the 51 largest orchestras in the United States, revealed 27% of its musicians had used beta blockers and 70% obtained them from friends, not physicians.[29] Beta blockers are inexpensive, said to be relatively safe, and on one hand, seem to improve musicians' performances on a technical level, while some, such as Barry Green, the author of "The Inner Game of Music" and Don Greene, a former Olympic diving coach who teaches Juilliard students to overcome their stage fright naturally, say the performances may be perceived as "soulless and inauthentic".[29]
Surgery
Low certainty evidence indicates that the use of beta blockers around the time of cardiac surgery may decrease the risk of heart dysrhythmias and atrial fibrillation.[30] Starting them around the time of other types of surgery, however, may worsen outcomes. For non-cardiac surgery, the use of beta blockers to prevent adverse effects may reduce the risk of atrial fibrillation and myocardial infarctions (very low certainty evidence), however, there is moderate certainty evidence that this approach may increase the risk of hypotension.[31] Low-certainty evidence suggests that beta blockers used perioperatively in non-cardiac surgeries may increase the risk of bradycardia.[31]
Other
A 2014 Cochrane review investigated the use of beta blockers in the maintenance of chronic type B thoracic aortic aneurysm in comparison to other anti hypertensive medications.[32] The review found no suitable evidence to support the current guidelines recommending its use.[32]
A 2017 Cochrane review on the use of beta blockers to prevent aortic dissections in people with Marfan syndrome was unable to draw definitive conclusions due to lack of evidence.[33]
Performance-enhancing use
Because they promote lower heart rates and reduce tremors, beta blockers have been used in professional sports where high accuracy is required, including archery, shooting, golf[34] and snooker.[34] Beta blockers are banned in some sports by the International Olympic Committee.[35] In the 2008 Summer Olympics, 50-metre pistol silver medalist and 10-metre air pistol bronze medalist Kim Jong-su tested positive for propranolol and was stripped of his medals.[36]
For similar reasons, beta blockers have also been used by surgeons.[37]
Classical musicians have commonly used beta blockers since the 1970s to reduce stage fright.[38]
Adverse effects
Adverse drug reactions associated with the use of beta blockers include: nausea, diarrhea, bronchospasm, dyspnea, cold extremities, exacerbation of Raynaud's syndrome, bradycardia, hypotension, heart failure, heart block, fatigue, dizziness, alopecia (hair loss), abnormal vision, hallucinations, insomnia, nightmares, sexual dysfunction, erectile dysfunction and/or alteration of glucose and lipid metabolism. Mixed α1/β-antagonist therapy is also commonly associated with orthostatic hypotension. Carvedilol therapy is commonly associated with edema.[39][page needed] Due to the high penetration across the blood–brain barrier, lipophilic beta blockers, such as propranolol and metoprolol, are more likely than other less lipophilic beta blockers to cause sleep disturbances, such as insomnia, vivid dreams and nightmares.[40]
Adverse effects associated with β2-adrenergic receptor antagonist activity (bronchospasm, peripheral vasoconstriction, alteration of glucose and lipid metabolism) are less common with β1-selective (often termed "cardioselective") agents, but receptor selectivity diminishes at higher doses. Beta blockade, especially of the beta-1 receptor at the macula densa, inhibits renin release, thus decreasing the release of aldosterone. This causes hyponatremia and hyperkalemia.[citation needed]
Hypoglycemia can occur with beta blockade because β2-adrenoceptors normally stimulate glycogen breakdown (glycogenolysis) in the liver and pancreatic release of the hormone glucagon, which work together to increase plasma glucose. Therefore, blocking β2-adrenoceptors lowers plasma glucose. β1-blockers have fewer metabolic side effects in diabetic patients; however, the fast heart rate that serves as a warning sign for insulin-induced low blood sugar may be masked, resulting in hypoglycemia unawareness. This is termed beta blocker-induced hypoglycemia unawareness. Therefore, beta blockers are to be used cautiously in diabetics.[41]
A 2007 study revealed diuretics and beta blockers used for hypertension increase a patient's risk of developing diabetes mellitus, while ACE inhibitors and angiotensin II receptor antagonists (angiotensin receptor blockers) actually decrease the risk of diabetes.[42] Clinical guidelines in Great Britain, but not in the United States, call for avoiding diuretics and beta blockers as first-line treatment of hypertension due to the risk of diabetes.[43]
Beta blockers must not be used in the treatment of selective alpha-adrenergic agonist overdose. The blockade of only beta receptors increases blood pressure, reduces coronary blood flow, left ventricular function, and cardiac output and tissue perfusion by means of leaving the alpha-adrenergic system stimulation unopposed. Beta blockers with lipophilic properties and CNS penetration such as metoprolol and labetalol may be useful for treating CNS and cardiovascular toxicity from a methamphetamine overdose.[44] The mixed alpha- and beta blocker labetalol is especially useful for treatment of concomitant tachycardia and hypertension induced by methamphetamine.[45] The phenomenon of "unopposed alpha stimulation" has not been reported with the use of beta blockers for treatment of methamphetamine toxicity.[45] Other appropriate antihypertensive drugs to administer during hypertensive crisis resulting from stimulant overdose are vasodilators such as nitroglycerin, diuretics such as furosemide, and alpha blockers such as phentolamine.[46]
Contraindications & cautions
Absolute contraindications:
- Bradycardia[47]
- Hypotension
- Hypersensitivity to beta blockers[47]
- Cardiogenic shock[47]
- Second or third degree AV block
Relative contraindications, or contraindications specific to certain beta-blockers:
- Long QT Syndrome: sotalol is contraindicated
- History of Torsades de Pointes: sotalol is contraindicated
Cautions:
- Abrupt discontinuations
- Acute bronchospasm[47]
- Acute heart failure[47]
- Asthma: see below
- Bronchitis[47]
- Cerebrovascular disease
- Chronic obstructive pulmonary disease (COPD)
- Emphysema[47]
- Kidney failure
- Hepatic disease
- Myopathy
- Pheochromocytoma
- Psoriasis
- Reynaud phenomenon
- Stroke
- Vasospastic angina
- Wolff–Parkinson–White syndrome[47]
Asthma
The 2007 National Heart, Lung, and Blood Institute (NHLBI) asthma guidelines recommend against the use of non-selective beta blockers in asthmatics, while allowing for the use of cardio selective beta blockers.[48]:182
Cardio selective beta blocker (β1 blockers) can be prescribed at the least possible dose to those with mild to moderate respiratory symptoms.[49][50] β2-agonists can somewhat mitigate β-blocker-induced bronchospasm where it exerts greater efficacy on reversing selective β-blocker-induced bronchospasm than the nonselective β-blocker-induced worsening asthma and/or COPD.[49]
Diabetes mellitus
Epinephrine signals early warning of the upcoming hypoglycemia.[51]
Beta blockers' inhibition on epinephrine's effect can somewhat exacerbate hypoglycemia by interfering with glycogenolysis and mask signs of hypoglycemia such as tachycardia, palpitations, diaphoresis, and tremors. Diligent blood glucose level monitoring is necessary for a patient with diabetes mellitus on beta blocker.
Hyperthyroidism
Abrupt withdrawal can result in a thyroid storm.[47]
Bradycardia or AV block
Unless a pacemaker is present, beta blockers can severely depress conduction in the AV node, resulting in a reduction of heart rate and cardiac output. One should be very cautious with the use of beta blockers in tachycardia patients with Wolff-Parkinson-White Syndrome, as it can result in life-threatening arrhythmia in certain patients. By slowing the conduction through the AV node, preferential conduction through the accessory pathway is favored. If the patient happens to develop atrial flutter, this could lead to a 1:1 conduction with very fast ventricular rate, or worse, ventricular fibrillation in the case of atrial fibrillation.[citation needed]
Toxicity
Glucagon, used in the treatment of overdose,[52][53] increases the strength of heart contractions, increases intracellular cAMP, and decreases renal vascular resistance. It is, therefore, useful in patients with beta blocker cardiotoxicity.[54][55] Cardiac pacing is usually reserved for patients unresponsive to pharmacological therapy.
People experiencing bronchospasm due to the β2 receptor-blocking effects of nonselective beta blockers may be treated with anticholinergic drugs, such as ipratropium, which are safer than beta agonists in patients with cardiovascular disease. Other antidotes for beta blocker poisoning are salbutamol and isoprenaline.
β-Adrenergic receptor antagonism
Stimulation of β1 receptors by epinephrine and norepinephrine induces a positive chronotropic and inotropic effect on the heart and increases cardiac conduction velocity and automaticity.[56] Stimulation of β1 receptors on the kidney causes renin release.[57] Stimulation of β2 receptors induces smooth muscle relaxation,[58] induces tremor in skeletal muscle,[59] and increases glycogenolysis in the liver and skeletal muscle.[60] Stimulation of β3 receptors induces lipolysis.[61]
Beta blockers inhibit these normal epinephrine- and norepinephrine-mediated sympathetic actions,[3] but have minimal effect on resting subjects.[citation needed] That is, they reduce the effect of excitement or physical exertion on heart rate and force of contraction,[62] and also tremor,[63] and breakdown of glycogen. Beta blockers can have a constricting effect on the bronchi of the lungs, possibly worsening or causing asthma symptoms.[64]
Since β2 adrenergic receptors can cause vascular smooth muscle dilation, beta blockers may cause some vasoconstriction. However, this effect tends to be small because the activity of β2 receptors is overshadowed by the more dominant vasoconstricting α1 receptors. By far the greatest effect of beta blockers remains in the heart. Newer, third-generation beta blockers can cause vasodilation through blockade of alpha-adrenergic receptors.[65]
Accordingly, nonselective beta blockers are expected to have antihypertensive effects.[66] The primary antihypertensive mechanism of beta blockers is unclear, but may involve reduction in cardiac output (due to negative chronotropic and inotropic effects).[67] It may also be due to reduction in renin release from the kidneys, and a central nervous system effect to reduce sympathetic activity (for those beta blockers that do cross the blood–brain barrier, e.g. propranolol).[citation needed]
Antianginal effects result from negative chronotropic and inotropic effects, which decrease cardiac workload and oxygen demand. Negative chronotropic properties of beta blockers allow the lifesaving property of heart rate control. Beta blockers are readily titrated to optimal rate control in many pathologic states.[citation needed]
The antiarrhythmic effects of beta blockers arise from sympathetic nervous system blockade—resulting in depression of sinus node function and atrioventricular node conduction, and prolonged atrial refractory periods. Sotalol, in particular, has additional antiarrhythmic properties and prolongs action potential duration through potassium channel blockade.
Blockade of the sympathetic nervous system on renin release leads to reduced aldosterone via the renin–angiotensin–aldosterone system, with a resultant decrease in blood pressure due to decreased sodium and water retention.
Additional pharmacological properties
Intrinsic sympathomimetic activity
Also referred to as intrinsic sympathomimetic effect, this term is used particularly with beta blockers that can show both agonism and antagonism at a given beta receptor, depending on the concentration of the agent (beta blocker) and the concentration of the antagonized agent (usually an endogenous compound, such as norepinephrine). See partial agonist for a more general description.[citation needed]
Some beta blockers (e.g. oxprenolol, pindolol, penbutolol, labetalol and acebutolol) exhibit intrinsic sympathomimetic activity (ISA). These agents are capable of exerting low-level agonist activity at the β-adrenergic receptor while simultaneously acting as a receptor site antagonist. These agents, therefore, may be useful in individuals exhibiting excessive bradycardia with sustained beta blocker therapy.[citation needed]
Agents with ISA should not be used for patients with any kind of angina as it can aggravate or after myocardial infarctions. They may also be less effective than other beta blockers in the management of angina and tachyarrhythmia.[39]
α1-Adrenergic receptor antagonism
Some beta blockers (e.g., labetalol and carvedilol) exhibit mixed antagonism of both β- and α1-adrenergic receptors, which provides additional arteriolar vasodilating action.[68][69]
Blood–brain barrier permeability
Beta blockers vary in their lipophilicity (fat solubility) and in turn in their ability to cross the blood–brain barrier and exert effects in the central nervous system.[70] Beta blockers with greater blood–brain barrier permeability can have both neuropsychiatric therapeutic benefits and side effects, as well as adverse cognitive effects.[70] Central nervous system-related side effects and risks of beta blockers may include fatigue, depression, sleep disorders (namely insomnia) and nightmares, visual hallucinations, delirium, psychosis, Parkinson's disease, and falling.[70] Conversely, central nervous system-related benefits of beta blockers may include prevention and treatment of migraine, essential tremor, akathisia, anxiety, post-traumatic stress disorder, aggression, and obsessive–compulsive disorder.[70]
Most beta blockers are lipophilic and can cross into the brain, but there are a number of exceptions.[70] Highly lipophilic beta blockers include penbutolol, pindolol, propranolol, and timolol, moderately lipophilic beta blockers include acebutolol, betaxolol, bisoprolol, carvedilol, metoprolol, and nebivolol, and low lipophilicity or hydrophilic beta blockers include atenolol, carteolol, esmolol, labetalol, nadolol, and sotalol.[70] It is thought that highly lipophilic beta blockers are able to readily cross into the brain, moderately lipophilic beta blockers are able to cross to a lesser degree, and low lipophilicity or hydrophilic beta blockers are minimally able to cross.[70] The preceding beta blockers also vary in their intrinsic sympathomimetic activity and β1-adrenergic receptor selectivity (or cardioselectivity), resulting in further differences in pharmacological profiles and suitability in different contexts between them.[70]
Examples

Nonselective agents
Nonselective beta blockers display both β1 and β2 antagonism.[71]
- Propranolol[71]
- Bucindolol (has additional α1-blocking activity)[72]
- Carteolol[73]
- Carvedilol (has additional α1-blocking activity)[71]
- Labetalol (has intrinsic sympathomimetic activity and additional α1-blocking activity)[71]
- Nadolol[71]
- Oxprenolol (has intrinsic sympathomimetic activity)[74]
- Penbutolol (has intrinsic sympathomimetic activity)[71]
- Pindolol (has intrinsic sympathomimetic activity)[71]
- Sotalol (not considered a "typical beta blocker")[71]
- Timolol[71]
β1-selective agents
β1-selective beta blockers are also known as cardioselective beta blockers.[71] Pharmacologically, the beta-blockade of the β1 receptors in the heart will act on cAMP. The function of cAMP as a second messenger in the cardiac cell is that it phosphorylates the LTCC and the ryanodine receptor to increase intracellular calcium levels and cause contraction. Beta-blockade of the β1 receptor will inhibit cAMP from phosphorylating, and it will decrease the ionotrophic and chronotropic effect. Note that drugs may be cardioselective, or act on β1 receptors in the heart only, but still have instrinsic sympathomimetic activity.
- Acebutolol (has intrinsic sympathomimetic activity, ISA)[71]
- Atenolol[71]
- Betaxolol[71]
- Bisoprolol[71]
- Celiprolol (has intrinsic sympathomimetic activity)[75]
- Metoprolol[71]
- Nebivolol[71]
- Esmolol[76]
Nebivolol and bisoprolol are the most β1 cardioselective beta blockers.[77]
β2-selective agents
β3-selective agents
β1 selective antagonist and β3 agonist agents
Comparative information
Pharmacological differences
- Agents with intrinsic sympathomimetic action (ISA)
- Agents organized by lipid solubility (lipophilicity)[83]
- High lipophilicity: propranolol, labetalol
- Intermediate lipophilicity: metoprolol, bisoprolol, carvedilol, acebutolol, timolol, pindolol
- Low lipophilicity (also known as hydrophilic beta blockers): atenolol, nadolol, and sotalol
- Agents with membrane stabilizing effect[84]
- Carvedilol, propranolol > oxprenolol > labetalol, metoprolol, timolol
Indication differences
- Agents specifically labeled for cardiac arrhythmia
- Agents specifically labeled for congestive heart failure[71]
- Agents specifically labeled for glaucoma
- Agents specifically labeled for myocardial infarction[71]
- Atenolol, metoprolol (immediate release), propranolol (immediate release), timolol, carvedilol (after left ventricular dysfunction), bisoprolol (preventive treatment before and primary treatment after heart attacks)
- Agents specifically labeled for migraine prophylaxis[89]
Propranolol is the only agent indicated for the control of tremor, portal hypertension, and esophageal variceal bleeding, and used in conjunction with α-blocker therapy in phaeochromocytoma.[39]
Other effects
Beta blockers, due to their antagonism at beta-1 adrenergic receptors, inhibit both the synthesis of new melatonin and its secretion by the pineal gland. The neuropsychiatric side effects of some beta blockers (e.g. sleep disruption, insomnia) may be due to this effect.[90]
Some pre-clinical and clinical research suggests that some beta blockers may be beneficial for cancer treatment.[91][92] However, other studies do not show a correlation between cancer survival and beta blocker usage.[93][94] Also, a 2017 meta-analysis failed to show any benefit for the use of beta blockers in breast cancer.[95]
Beta blockers have also been used for the treatment of schizoid personality disorder.[96] However, there is limited evidence supporting the efficacy of supplemental beta blocker use in addition to antipsychotic drugs for treating schizophrenia.[97][98]
Contrast agents are not contraindicated in those receiving beta blockers.[99]
See also
- Alpha blockers
References
- ↑ "beta Blockade after myocardial infarction: systematic review and meta regression analysis". BMJ 318 (7200): 1730–1737. June 1999. doi:10.1136/bmj.318.7200.1730. PMID 10381708.
- ↑ "2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8)". JAMA 311 (5): 507–520. February 2014. doi:10.1001/jama.2013.284427. PMID 24352797.
- ↑ 3.0 3.1 3.2 "Beta-Adrenergic Blockers". Current Cardiovascular Drugs. Current Science Group. 2005. ISBN 978-1-57340-221-7. https://books.google.com/books?id=y3R1Vd3NHqcC&q=mode+of+action+of+beta+blockers&pg=PA152. Retrieved 2010-09-07.
- ↑ 4.0 4.1 4.2 "Hypertension". Pharmacotherapeutics for advanced practice: a practical approach. Lippincott Williams & Wilkins. 2006. p. 205. ISBN 978-0-7817-5784-3. https://books.google.com/books?id=EaP1yJz4fkEC&pg=PA205. Retrieved 2010-09-07.
- ↑ "Genetic variation in the beta 3-adrenergic receptor and an increased capacity to gain weight in patients with morbid obesity". The New England Journal of Medicine 333 (6): 352–354. August 1995. doi:10.1056/NEJM199508103330605. PMID 7609752.
- ↑ "Sir James Black, OM". The Telegraph. 23 March 2010. https://www.telegraph.co.uk/news/obituaries/medicine-obituaries/7507080/Sir-James-Black-OM.html.
- ↑ "Combination of calcium channel blockers and beta blockers for patients with exercise-induced angina pectoris: a double-blind parallel-group comparison of different classes of calcium channel blockers. The Netherlands Working Group on Cardiovascular Research (WCN)". Angiology 50 (6): 447–454. June 1999. doi:10.1177/000331979905000602. PMID 10378820.
- ↑ "Sir James Black and propranolol. The role of the basic sciences in the history of cardiovascular pharmacology". Texas Heart Institute Journal 24 (4): 336–342. 1997. PMID 9456487.
- ↑ "Beta-blockers for hypertension". The Cochrane Database of Systematic Reviews 1 (1): CD002003. January 2017. doi:10.1002/14651858.CD002003.pub5. PMID 28107561.
- ↑ Reinhart, Marcia; Puil, Lorri; Salzwedel, Douglas M.; Wright, James M. (2023-07-13). "First-line diuretics versus other classes of antihypertensive drugs for hypertension". The Cochrane Database of Systematic Reviews 7 (7): CD008161. doi:10.1002/14651858.CD008161.pub3. ISSN 1469-493X. PMID 37439548. PMC 10339786. https://pubmed.ncbi.nlm.nih.gov/37439548.
- ↑ "Calcium channel blockers versus other classes of drugs for hypertension". The Cochrane Database of Systematic Reviews 1 (1): CD003654. January 2022. doi:10.1002/14651858.CD003654.pub6. PMID 35000192.
- ↑ "Beta-blockers for hypertension". The Cochrane Database of Systematic Reviews 1 (1): CD002003. January 2017. doi:10.1002/14651858.cd002003.pub5. PMID 28107561.
- ↑ Drugs for the Heart. Philadelphia: Saunders. 2009. pp. 6–18. ISBN 978-1-4160-6158-8.
- ↑ "Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: the Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT-HF). MERIT-HF Study Group". JAMA 283 (10): 1295–1302. March 2000. doi:10.1001/jama.283.10.1295. PMID 10714728.
- ↑ "Bisoprolol for the treatment of chronic heart failure: a meta-analysis on individual data of two placebo-controlled studies--CIBIS and CIBIS II. Cardiac Insufficiency Bisoprolol Study". American Heart Journal 143 (2): 301–307. February 2002. doi:10.1067/mhj.2002.120768. PMID 11835035.
- ↑ "Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study". Circulation 106 (17): 2194–2199. October 2002. doi:10.1161/01.CIR.0000035653.72855.BF. PMID 12390947.
- ↑ "Beta blockers in heart failure" (in en). Australian Prescriber 23 (6): 120–123. 2000. doi:10.18773/austprescr.2000.138. https://www.nps.org.au/australian-prescriber/articles/beta-blockers-in-heart-failure.
- ↑ "Use of beta-blockers and ivabradine in heart failure with reduced ejection fraction". http://www.uptodate.com/contents/use-of-beta-blockers-and-ivabradine-in-heart-failure-with-reduced-ejection-fraction.
- ↑ "Beta-blockers: new standard therapy for heart failure". Mayo Clinic Proceedings 77 (8): 839–45; quiz 845–46. August 2002. doi:10.4065/77.8.839. PMID 12173717.
- ↑ "Beta-blockers for congestive heart failure in children". The Cochrane Database of Systematic Reviews 7 (7): CD007037. July 2020. doi:10.1002/14651858.CD007037.pub4. PMID 32700759.
- ↑ Goodman & Gilman's: The Pharmacological Basic of Therapeutics. McGraw-Hill. 2018. ISBN 9781259584732.
- ↑ 22.0 22.1 22.2 22.3 22.4 "Beta-blockers for suspected or diagnosed acute myocardial infarction". The Cochrane Database of Systematic Reviews 12 (12): CD012484. December 2019. doi:10.1002/14651858.CD012484.pub2. PMID 31845756.
- ↑ 23.0 23.1 "Beta Blockers". StatPearls. Treasure Island (FL): StatPearls Publishing. 2023. http://www.ncbi.nlm.nih.gov/books/NBK532906/. Retrieved 2023-10-31.
- ↑ "Essential Hypertension". StatPearls. Treasure Island (FL): StatPearls Publishing. 2023. http://www.ncbi.nlm.nih.gov/books/NBK539859/. Retrieved 2023-10-31.
- ↑ 25.0 25.1 "Blood pressure lowering efficacy of nonselective beta-blockers for primary hypertension". The Cochrane Database of Systematic Reviews 2014 (2): CD007452. February 2014. doi:10.1002/14651858.CD007452.pub2. PMID 24585007.
- ↑ 26.0 26.1 "Beta-blockers for hypertension". The Cochrane Database of Systematic Reviews 1 (1): CD002003. January 2017. doi:10.1002/14651858.CD002003.pub5. PMID 28107561..
- ↑ "Clinical practice. Social anxiety disorder". The New England Journal of Medicine 355 (10): 1029–1036. September 2006. doi:10.1056/NEJMcp060145. PMID 16957148.
- ↑ "Anxiolytics not acting at the benzodiazepine receptor: beta blockers". Progress in Neuro-Psychopharmacology & Biological Psychiatry 16 (1): 17–26. January 1992. doi:10.1016/0278-5846(92)90004-X. PMID 1348368.
- ↑ 29.0 29.1 "Better Playing Through Chemistry". The New York Times. October 17, 2004. https://www.nytimes.com/2004/10/17/arts/music/better-playing-through-chemistry.html.
- ↑ "Perioperative beta-blockers for preventing surgery-related mortality and morbidity in adults undergoing cardiac surgery". The Cochrane Database of Systematic Reviews 9 (9): CD013435. September 2019. doi:10.1002/14651858.CD013435. PMID 31544227.
- ↑ 31.0 31.1 "Perioperative beta-blockers for preventing surgery-related mortality and morbidity in adults undergoing non-cardiac surgery". The Cochrane Database of Systematic Reviews 2019 (9): CD013438. September 2019. doi:10.1002/14651858.CD013438. PMID 31556094.
- ↑ 32.0 32.1 "First-line beta-blockers versus other antihypertensive medications for chronic type B aortic dissection". The Cochrane Database of Systematic Reviews (2): CD010426. February 2014. doi:10.1002/14651858.CD010426.pub2. PMID 24570114.
- ↑ "Beta-blockers for preventing aortic dissection in Marfan syndrome". The Cochrane Database of Systematic Reviews 11 (11): CD011103. November 2017. doi:10.1002/14651858.CD011103.pub2. PMID 29110304.
- ↑ 34.0 34.1 Tim Glover. "Golf: O'Grady says players use beta-blockers: Drugs 'helped win majors'". The Independent. https://www.independent.co.uk/sport/golf-ogrady-says-players-use-betablockers-drugs-helped-win-majors-1368307.html.
- ↑ World Anti-Doping Agency (September 19, 2005). "The World Anti-Doping Code: The 2006 Prohibited List International Standard". World Anti-Doping Agency. https://www.wada-ama.org/sites/default/files/resources/files/WADA_Prohibited_List_2006_EN.pdf.
- ↑ "Olympics: North Korea's Kim Jong-su loses medals after positive drugs test" (in en). The Guardian (Guardian News and Media Limited). 15 August 2008. https://www.theguardian.com/sport/2008/aug/15/olympics2008.drugsinsport.
- ↑ "The effect of propranolol versus placebo on resident surgical performance". Transactions of the American Ophthalmological Society 96: 283–91; discussion 291–4. 1998. PMID 10360293.
- ↑ "Musicians Use Beta Blockers as Performance-Enabling Drugs". WQXR. August 16, 2013. https://www.wqxr.org/story/312920-musicians-use-beta-blockers-relieve-stage-fright/.
- ↑ 39.0 39.1 39.2 Rossi S, ed (2006). Australian Medicines Handbook. Adelaide: Australian Medicines Handbook.
- ↑ "Beta-blockers and heart failure". Indian Heart Journal 62 (2): 101–110. 2010. PMID 21180298.
- ↑ Beta-Adrenoceptor Antagonists (Beta-Blockers); "Beta-Adrenoceptor Antagonists (Beta-Blockers)". CV Pharmacology. http://www.cvpharmacology.com/cardioinhibitory/beta-blockers.htm.
- ↑ "Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis". Lancet 369 (9557): 201–207. January 2007. doi:10.1016/S0140-6736(07)60108-1. PMID 17240286.
- ↑ "NICE removes beta blockers as first line treatment for hypertension". BMJ 333 (7557): 8. July 2006. doi:10.1136/bmj.333.7557.8-a. PMID 16809680.
- ↑ "Methamphetamine Toxicity: Treatment & Management". Medscape. WebMD. http://emedicine.medscape.com/article/820918-overview#showall.
- ↑ 45.0 45.1 "Treatment of toxicity from amphetamines, related derivatives, and analogues: a systematic clinical review". Drug and Alcohol Dependence 150: 1–13. May 2015. doi:10.1016/j.drugalcdep.2015.01.040. PMID 25724076.
- ↑ "Toxicity, Amphetamine". Medscape. 16 December 2016. http://www.emedicine.com/EMERG/topic23.htm.
- ↑ 47.0 47.1 47.2 47.3 47.4 47.5 47.6 47.7 47.8 Wyeth Pharmaceuticals Inc.. "Propranolol hydrochloride". https://www.accessdata.fda.gov/drugsatfda_docs/label/2007/016418s078lbl.pdf.
- ↑ "Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma–Summary Report 2007". The Journal of Allergy and Clinical Immunology 120 (5): S94–S138. 2007. doi:10.1016/j.jaci.2007.09.029. https://www.jacionline.org/article/S0091-6749(07)01823-4/fulltext. Retrieved 2017-12-09.
- ↑ 49.0 49.1 "Adverse respiratory effect of acute β-blocker exposure in asthma: a systematic review and meta-analysis of randomized controlled trials". Chest (Elsevier BV) 145 (4): 779–786. April 2014. doi:10.1378/chest.13-1235. PMID 24202435.
- ↑ "Cardioselective beta-blockers in patients with reactive airway disease: a meta-analysis". Annals of Internal Medicine (American College of Physicians) 137 (9): 715–725. November 2002. doi:10.7326/0003-4819-137-9-200211050-00035. PMID 12416945.
- ↑ "Glucose counterregulatory responses to hypoglycemia". Pediatric Endocrinology Reviews 9 (1): 463–475. September 2011. PMID 22783644.
- ↑ "Beta blocker overdose with propranolol and with atenolol". Annals of Emergency Medicine 14 (2): 161–163. February 1985. doi:10.1016/S0196-0644(85)81081-7. PMID 2857542.
- ↑ "Toxicity, Beta-blocker: Treatment & Medication – eMedicine Emergency Medicine". http://emedicine.medscape.com/article/813342-treatment.
- ↑ John Gualtier. "Beta-Adrenergic Blocker Poisoning". http://www.courses.ahc.umn.edu/pharmacy/6124/handouts/Beta%20blockers.pdf.
- ↑ USMLE WORLD 2009 Step1, Pharmacology, Q85
- ↑ "Adrenergic Receptors in Clinical Medicine". The Adrenergic Receptors in the 21st Century. Humana Press. 2006. p. 135. ISBN 978-1-58829-423-4. https://books.google.com/books?id=QNpIsKwp8PUC&q=%CE%B21+receptors+positive+chronotropic+inotropic+effect&pg=PA135. Retrieved 2010-09-08.[yes|permanent dead link|dead link}}]
- ↑ Harrison's Nephrology and Acid-Base Disorders. McGraw-Hill Companies. 2010. p. 215. ISBN 978-0-07-166339-7. https://books.google.com/books?id=zVQZpJnQM_AC&q=%CE%B21+receptors+kidneys+renin&pg=PA215. Retrieved 2010-09-08.
- ↑ "Vasoactive Amines and Inotropic Agents". Surgical Intensive Care Medicine. Springer. 2009. p. 47. ISBN 978-0-387-77892-1. https://books.google.com/books?id=Bih5AXq_0uMC&q=b2+receptors+smooth+muscle+relaxation&pg=PA47. Retrieved 2010-09-08.
- ↑ "Skeletal muscle tremor and the influence of adrenergic drugs". The Journal of Asthma 27 (1): 11–20. 1990. doi:10.3109/02770909009073289. PMID 1968452.
- ↑ Sport and exercise pharmacology. Human Kinetics. 2000. p. 19. ISBN 978-0-87322-937-1. https://books.google.com/books?id=8ysOZlGnkC0C&q=beta+blocker+stimulation+glycogenolysis&pg=PA19. Retrieved 2010-09-10.
- ↑ Anatomy and Physiology. Pearson Education. 2005. p. 394. ISBN 978-0-8053-5947-3. https://books.google.com/books?id=0e08PrEMQJoC&q=beta+3+stimulating+lipolysis&pg=PA394. Retrieved 2010-09-10.
- ↑ "Beta-Blockers". Encyclopedia of Heart Diseases. Elsevier. 2006. p. 160. ISBN 978-0-12-406061-6. https://books.google.com/books?id=xco9aJ_Y9XIC&q=beta+blockers+effects+on+heart+rate&pg=PA160. Retrieved 2010-09-10.
- ↑ Improving Oral Health for the Elderly: An Interdisciplinary Approach. New York: Springer. 2008. p. 87. ISBN 978-0-387-74337-0. https://books.google.com/books?id=qs2v9Sm-dVoC&q=beta+blockers+reduce+tremor&pg=PA87. Retrieved 2010-10-23.
- ↑ "Beta Antagonist (Blocker) Medications". The Encyclopedia of Men's Health. Amaranth. 2005. p. 48. ISBN 978-0-8160-5177-9. https://books.google.com/books?id=AyPacn1o4nIC&q=beta+blockers+opening+of+bronchi&pg=PA48. Retrieved 2010-10-23.
- ↑ 100 Questions and Answers about Hypertension. Blackwell Science. 2001. p. 106. ISBN 978-0-632-04481-8. https://archive.org/details/100questionsansw0000mang. Retrieved 2010-09-10. "beta blockers dilation of blood vessels."
- ↑ "Hypertension: Epidemiology, Pathophysiology, Diagnosis and Treatment". Hurst's the Heart. 2. Blackwell Science.. 1997. p. 1564. ISBN 978-0-07-912951-2. https://books.google.com/books?id=eWQAJDrVV7gC&q=beta+blockers+antihypertensive&pg=PA1564. Retrieved 2010-10-07.
- ↑ Lecture notes on clinical pharmacology. 6. Blackwell Science.. 2001. p. 76. ISBN 978-0-632-05077-2. https://books.google.com/books?id=dsEmlotDt2wC&q=beta+blockers+antihypertensive+effect+reduction+of+cardiac+output&pg=PA76. Retrieved 2011-03-11.
- ↑ "Labetalol Hydrochloride Monograph for Professionals". American Society of Health-System Pharmacists. https://www.drugs.com/monograph/labetalol-hydrochloride.html.
- ↑ "Coreg - Food and Drug Administration". http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020297s029lbl.pdf.
- ↑ 70.0 70.1 70.2 70.3 70.4 70.5 70.6 70.7 "Neuropsychiatric Consequences of Lipophilic Beta-Blockers". Medicina 57 (2): 155. February 2021. doi:10.3390/medicina57020155. PMID 33572109.
- ↑ 71.00 71.01 71.02 71.03 71.04 71.05 71.06 71.07 71.08 71.09 71.10 71.11 71.12 71.13 71.14 71.15 71.16 71.17 71.18 71.19 "Comparison of Oral Beta-Blockers". Therapeutic Research Center. https://pharmacist.therapeuticresearch.com/Content/Segments/PRL/2012/Dec/Comparison-of-Oral-Beta-Blockers-5052.
- ↑ "Beta-blocking agents with vasodilator activity". Journal of Hypertension. Supplement 11 (4): S37–S40. June 1993. doi:10.1097/00004872-199306003-00009. PMID 8104240.
- ↑ "CARTEOLOL" (in en). U.S. National Library of Medicine. https://pubchem.ncbi.nlm.nih.gov/compound/carteolol.
- ↑ 74.0 74.1 "oxprenolol" (in en). U.S. National Library of Medicine. https://pubchem.ncbi.nlm.nih.gov/compound/4631.
- ↑ 75.0 75.1 "Celiprolol" (in en). U.S. National Library of Medicine. https://pubchem.ncbi.nlm.nih.gov/compound/2663.
- ↑ "Esmolol, an ultrashort-acting, selective beta 1-adrenoceptor antagonist: pharmacodynamic and pharmacokinetic properties". European Journal of Clinical Pharmacology 46 (5): 399–404. 1994. doi:10.1007/BF00191900. PMID 7957532.
- ↑ "The double jeopardy of chronic obstructive pulmonary disease and myocardial infarction". Open Heart 1 (1): e000010. February 2014. doi:10.1136/openhrt-2013-000010. PMID 25332777.
- ↑ "Butaxamine" (in en). U.S. National Library of Medicine. https://pubchem.ncbi.nlm.nih.gov/compound/18026.
- ↑ "ICI 118551" (in en). https://www.ebi.ac.uk/chebi/searchId.do?chebiId=CHEBI%3A73289.
- ↑ "SR 59230A" (in en). U.S. National Library of Medicine. https://pubchem.ncbi.nlm.nih.gov/compound/9888075.
- ↑ 81.0 81.1 81.2 "β-Blockers in hypertension: studies and meta-analyses over the years". The Canadian Journal of Cardiology 30 (5 Suppl): S16–S22. May 2014. doi:10.1016/j.cjca.2014.02.012. PMID 24750978.
- ↑ Pharmacology of Antihypertensive Therapeutics. Berlin, Heidelberg: Springer Berlin Heidelberg. 1990. p. 523. ISBN 9783642742095.
- ↑ "Lipophilic β-Blockers and Suicide in the Elderly". Journal of Clinical Psychopharmacology 37 (3): 381–384. June 2017. doi:10.1097/JCP.0000000000000695. PMID 28338548.
- ↑ 84.0 84.1 84.2 84.3 84.4 "Changing beta-blockers in heart failure: when is a class not a class?". The British Journal of General Practice 58 (551): 387–389. June 2008. doi:10.3399/bjgp08X299317. PMID 18505613.
- ↑ "DailyMed - BREVIBLOC- esmolol hydrochloride injection". DailyMed. U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=595cc3d5-1306-4828-aefa-5595219ffd62.
- ↑ "DailyMed - BETAPACE- sotalol hydrochloride tablet BETAPACE AF- sotalol hydrochloride tablet". DailyMed. U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=afce2787-8899-4098-87c8-f1e8dd19e6dd.
- ↑ "Announcement of Approval of Additional Indications for Onoact 50 for Injection, Short-Acting Selective ß1 Blocker". Evaluate Ltd.. http://www.evaluategroup.com/Universal/View.aspx?type=Story&id=103244.
- ↑ "Metiprapanol – metipranolol solution/ drops". DailyMed. U.S. National Library of Medicine – NIH. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=699ce415-0798-4244-b5ec-bcdb383b50b3.
- ↑ "Drugs to Prevent Migraine in Adults". Therapeutic Research Center. https://pharmacist.therapeuticresearch.com/Content/Segments/PRL/2012/Jul/Drugs-to-Prevent-Migraine-in-Adults-4513.
- ↑ "Night-time exogenous melatonin administration may be a beneficial treatment for sleeping disorders in beta blocker patients". Journal of Cardiovascular Disease Research 2 (3): 153–155. July 2011. doi:10.4103/0975-3583.85261. PMID 22022142.
- ↑ "Inhibition of β2-adrenergic receptor reduces triple-negative breast cancer brain metastases: The potential benefit of perioperative β-blockade". Oncology Reports 35 (6): 3135–3142. June 2016. doi:10.3892/or.2016.4710. PMID 27035124.
- ↑ "Beta blocker use correlates with better overall survival in metastatic melanoma patients and improves the efficacy of immunotherapies in mice". Oncoimmunology 7 (3): e1405205. 2018. doi:10.1080/2162402X.2017.1405205. PMID 29399407.
- ↑ "β-Blocker use and all-cause mortality of melanoma patients: results from a population-based Dutch cohort study". European Journal of Cancer 49 (18): 3863–3871. December 2013. doi:10.1016/j.ejca.2013.07.141. PMID 23942335.
- ↑ "Beta-blocker usage and prostate cancer survival: a nested case-control study in the UK Clinical Practice Research Datalink cohort". Cancer Epidemiology 38 (3): 279–285. June 2014. doi:10.1016/j.canep.2014.03.011. PMID 24786858.
- ↑ "Is Beta-Blocker Use Beneficial in Breast Cancer? A Meta-Analysis". Oncology 92 (5): 264–268. 2017. doi:10.1159/000455143. PMID 28132057.
- ↑ ", Chapter 3, Schizoid Personality Disorder.". Personality Disorders: New Symptom-Focused Drug Therapy.. Psychology Press. 1997. pp. 45–56. ISBN 9780789001344.
- ↑ Cheine, M.; Ahonen, J.; Wahlbeck, K. (2001). "Beta-blocker supplementation of standard drug treatment for schizophrenia". The Cochrane Database of Systematic Reviews (3): CD000234. doi:10.1002/14651858.CD000234. ISSN 1469-493X. PMID 11686955. https://pubmed.ncbi.nlm.nih.gov/11686955.
- ↑ "Beta‐blocker supplementation of standard drug treatment for schizophrenia.". Cochrane Database of Systematic Reviews 2010 (7). September 1996. doi:10.1002/14651858.CD000234. https://www.cochrane.org/CD000234/SCHIZ_beta-blocker-supplementation-of-standard-drug-treatment-for-people-with-schizophrenia.
- ↑ "Beta blockers and intravenous roentgen contrast materials: Which risks do exist?". European Journal of Internal Medicine 35: e17–e18. November 2016. doi:10.1016/j.ejim.2016.08.003. PMID 27531627.
External links
- Musicians and beta-blockers by Gerald Klickstein, March 11, 2010 (A blog post that considers "whether beta-blockers are safe, effective, and appropriate for performers to use.")
- Better Playing Through Chemistry by Blair Tindall, The New York Times , October 17, 2004. (Discusses the use of beta blockers among professional musicians)
- Musicians using beta blockers by Blair Tindall. A condensed version of the above article.
- In Defense of the Beta Blocker by Carl Elliott, The Atlantic, August 20, 2008. (Discusses the use of propranolol by a North Korean pistol shooter in the 2008 Olympics)
- beta-Adrenergic+Blockers at the US National Library of Medicine Medical Subject Headings (MeSH)
 |

