Chemistry:Fat
| Types of fat]]s in food |
|---|
| See also |
In nutrition, biology, and chemistry, fat usually means any ester of fatty acids, or a mixture of such compounds, most commonly those that occur in living beings or in food.[1]
The term often refers specifically to triglycerides (triple esters of glycerol), that are the main components of vegetable oils and of fatty tissue in animals;[2] or, even more narrowly, to triglycerides that are solid or semisolid at room temperature, thus excluding oils. The term may also be used more broadly as a synonym of lipid—any substance of biological relevance, composed of carbon, hydrogen, or oxygen, that is insoluble in water but soluble in non-polar solvents.[1] In this sense, besides the triglycerides, the term would include several other types of compounds like mono- and diglycerides, phospholipids (such as lecithin), sterols (such as cholesterol), waxes (such as beeswax),[1] and free fatty acids, which are usually present in human diet in smaller amounts.[2]
Fats are one of the three main macronutrient groups in human diet, along with carbohydrates and proteins,[1][3] and the main components of common food products like milk, butter, tallow, lard, salt pork, and cooking oils. They are a major and dense source of food energy for many animals and play important structural and metabolic functions, in most living beings, including energy storage, waterproofing, and thermal insulation.[4] The human body can produce the fat it requires from other food ingredients, except for a few essential fatty acids that must be included in the diet. Dietary fats are also the carriers of some flavor and aroma ingredients and vitamins that are not water-soluble.[2]
Biological importance
In humans and many animals, fats serve both as energy sources and as stores for energy in excess of what the body needs immediately. Each gram of fat when burned or metabolized releases about 9 food calories (37 kJ = 8.8 kcal).[5]
Fats are also sources of essential fatty acids, an important dietary requirement. Vitamins A, D, E, and K are fat-soluble, meaning they can only be digested, absorbed, and transported in conjunction with fats.
Fats play a vital role in maintaining healthy skin and hair, insulating body organs against shock, maintaining body temperature, and promoting healthy cell function. Fat also serves as a useful buffer against a host of diseases. When a particular substance, whether chemical or biotic, reaches unsafe levels in the bloodstream, the body can effectively dilute—or at least maintain equilibrium of—the offending substances by storing it in new fat tissue.[6] This helps to protect vital organs, until such time as the offending substances can be metabolized or removed from the body by such means as excretion, urination, accidental or intentional bloodletting, sebum excretion, and hair growth.
Adipose tissue
In animals, adipose tissue, or fatty tissue is the body's means of storing metabolic energy over extended periods of time. Adipocytes (fat cells) store fat derived from the diet and from liver metabolism. Under energy stress these cells may degrade their stored fat to supply fatty acids and also glycerol to the circulation. These metabolic activities are regulated by several hormones (e.g., insulin, glucagon and epinephrine). Adipose tissue also secretes the hormone leptin.[7]
Production and processing
A variety of chemical and physical techniques are used for the production and processing of fats, both industrially and in cottage or home settings. They include:
- Pressing to extract liquid fats from fruits, seeds, or algae, e.g. olive oil from olives
- Solvent extraction using solvents like hexane or supercritical carbon dioxide
- Rendering, the melting of fat in adipose tissue, e.g. to produce tallow, lard, fish oil, and whale oil
- Churning of milk to produce butter
- Hydrogenation to increase the degree of saturation of the fatty acids
- Interesterification, the rearrangement of fatty acids across different triglycerides
- Winterization to remove oil components with higher melting points
- Clarification of butter
Metabolism
The pancreatic lipase acts at the ester bond, hydrolyzing the bond and "releasing" the fatty acid. In triglyceride form, lipids cannot be absorbed by the duodenum. Fatty acids, monoglycerides (one glycerol, one fatty acid), and some diglycerides are absorbed by the duodenum, once the triglycerides have been broken down.
In the intestine, following the secretion of lipases and bile, triglycerides are split into monoacylglycerol and free fatty acids in a process called lipolysis. They are subsequently moved to absorptive enterocyte cells lining the intestines. The triglycerides are rebuilt in the enterocytes from their fragments and packaged together with cholesterol and proteins to form chylomicrons. These are excreted from the cells and collected by the lymph system and transported to the large vessels near the heart before being mixed into the blood. Various tissues can capture the chylomicrons, releasing the triglycerides to be used as a source of energy. Liver cells can synthesize and store triglycerides. When the body requires fatty acids as an energy source, the hormone glucagon signals the breakdown of the triglycerides by hormone-sensitive lipase to release free fatty acids. As the brain cannot utilize fatty acids as an energy source (unless converted to a ketone),[8] the glycerol component of triglycerides can be converted into glucose, via gluconeogenesis by conversion into dihydroxyacetone phosphate and then into glyceraldehyde 3-phosphate, for brain fuel when it is broken down. Fat cells may also be broken down for that reason if the brain's needs ever outweigh the body's.
Triglycerides cannot pass through cell membranes freely. Special enzymes on the walls of blood vessels called lipoprotein lipases must break down triglycerides into free fatty acids and glycerol. Fatty acids can then be taken up by cells via fatty acid transport proteins (FATPs).
Triglycerides, as major components of very-low-density lipoprotein (VLDL) and chylomicrons, play an important role in metabolism as energy sources and transporters of dietary fat. They contain more than twice as much energy (approximately 9 kcal/g or 38 kJ/g) as carbohydrates (approximately 4 kcal/g or 17 kJ/g).[9]
Nutritional and health aspects
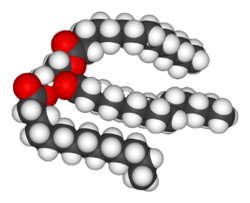
The most common type of fat, in human diet and most living beings, is a triglyceride, an ester of the triple alcohol glycerol H(–CHOH–)3H and three fatty acids. The molecule of a triglyceride can be described as resulting from a condensation reaction (specifically, esterification) between each of glycerol's –OH groups and the HO– part of the carboxyl group HO(O=)C– of each fatty acid, forming an ester bridge –O–(O=)C– with elimination of a water molecule H2O.
Other less common types of fats include diglycerides and monoglycerides, where the esterification is limited to two or just one of glycerol's –OH groups. Other alcohols, such as cetyl alcohol (predominant in spermaceti), may replace glycerol. In the phospholipids, one of the fatty acids is replaced by phosphoric acid or a monoester thereof. The benefits and risks of various amounts and types of dietary fats have been the object of much study, and are still highly controversial topics.[10][11][12][13]
Essential fatty acids
There are two essential fatty acids (EFAs) in human nutrition: alpha-Linolenic acid (an omega-3 fatty acid) and linoleic acid (an omega-6 fatty acid).[14][5] The adult body can synthesize other lipids that it needs from these two.
Dietary sources
Saturated vs. unsaturated fats
Different foods contain different amounts of fat with different proportions of saturated and unsaturated fatty acids. Some animal products, like beef and dairy products made with whole or reduced fat milk like yogurt, ice cream, cheese and butter have mostly saturated fatty acids (and some have significant contents of dietary cholesterol). Other animal products, like pork, poultry, eggs, and seafood have mostly unsaturated fats. Industrialized baked goods may use fats with high unsaturated fat contents as well, especially those containing partially hydrogenated oils, and processed foods that are deep-fried in hydrogenated oil are high in saturated fat content.[15][16][17]
Plants and fish oil generally contain a higher proportion of unsaturated acids, although there are exceptions such as coconut oil and palm kernel oil.[18][19] Foods containing unsaturated fats include avocado, nuts, olive oils, and vegetable oils such as canola.
Many careful studies have found that replacing saturated fats with cis unsaturated fats in the diet reduces risk of cardiovascular diseases (CVDs),[20][21] diabetes, or death.[22] These studies prompted many medical organizations and public health departments, including the World Health Organization (WHO),[23][24] to officially issue that advice. Some countries with such recommendations include:
- United Kingdom[25][26][27][28][29]
- United States[22][30][31][32][33]
- India[34][35]
- Canada[36]
- Australia[37]
- Singapore[38]
- New Zealand[39]
- Hong Kong[40]
A 2004 review concluded that "no lower safe limit of specific saturated fatty acid intakes has been identified" and recommended that the influence of varying saturated fatty acid intakes against a background of different individual lifestyles and genetic backgrounds should be the focus in future studies.[41]
This advice is often oversimplified by labeling the two kinds of fats as bad fats and good fats, respectively. However, since the fats and oils in most natural and traditionally processed foods contain both unsaturated and saturated fatty acids,[42] the complete exclusion of saturated fat is unrealistic and possibly unwise. For instance, some foods rich in saturated fat, such as coconut and palm oil, are an important source of cheap dietary calories for a large fraction of the population in developing countries.[43]
Concerns were also expressed at a 2010 conference of the American Dietetic Association that a blanket recommendation to avoid saturated fats could drive people to also reduce the amount of polyunsaturated fats, which may have health benefits, and/or replace fats by refined carbohydrates — which carry a high risk of obesity and heart disease.[44]
For these reasons, the U.S. Food and Drug Administration, for example, recommends to consume at least 10% (7% for high-risk groups) of calories from saturated fat, with an average of 30% (or less) of total calories from all fat.[45][43] A general 7% limit was recommended also by the American Heart Association (AHA) in 2006.[46][47]
The WHO/FAO report also recommended replacing fats so as to reduce the content of myristic and palmitic acids, specifically.[43]
The so-called Mediterranean diet, prevalent in many countries in the Mediterranean Sea area, includes more total fat than the diet of Northern European countries, but most of it is in the form of unsaturated fatty acids (specifically, monounsaturated and omega-3) from olive oil and fish, vegetables, and certain meats like lamb, while consumption of saturated fat is minimal in comparison. A 2017 review found evidence that a Mediterranean-style diet could reduce the risk of cardiovascular diseases, overall cancer incidence, neurodegenerative diseases, diabetes, and mortality rate.[48] A 2018 review showed that a Mediterranean-like diet may improve overall health status, such as reduced risk of non-communicable diseases. It also may reduce the social and economic costs of diet-related illnesses.[49]
A small number of contemporary reviews have challenged this negative view of saturated fats. For example, an evaluation of evidence from 1966 to 1973 of the observed health impact of replacing dietary saturated fat with linoleic acid found that it increased rates of death from all causes, coronary heart disease, and cardiovascular disease.[50] These studies have been disputed by many scientists,[51] and the consensus in the medical community is that saturated fat and cardiovascular disease are closely related.[52][53][54] Still, these discordant studies fueled debate over the merits of substituting polyunsaturated fats for saturated fats.[55]
Cardiovascular disease
The effect of saturated fat on cardiovascular disease has been extensively studied.[56] The general consensus is that there is evidence of moderate-quality of a strong, consistent, and graded relationship between saturated fat intake, blood cholesterol levels, and the incidence of cardiovascular disease.[22][56] The relationships are accepted as causal,[57][58] including by many government and medical organizations.[43][59][60][22][61][62][63][64]
A 2017 review by the AHA estimated that replacement of saturated fat with polyunsaturated fat in the American diet could reduce the risk of cardiovascular diseases by 30%.[22]
The consumption of saturated fat is generally considered a risk factor for dyslipidemia—abnormal blood lipid levels, including high total cholesterol, high levels of triglycerides, high levels of low-density lipoprotein (LDL, "bad" cholesterol) or low levels of high-density lipoprotein (HDL, "good" cholesterol). These parameters in turn are believed to be risk indicators for some types of cardiovascular disease.[65][66][67][68][69][61][70][71][72] These effects were observed in children too.[73]
Several meta-analyses (reviews and consolidations of multiple previously published experimental studies) have confirmed a significant relationship between saturated fat and high serum cholesterol levels,[22][74] which in turn have been claimed to have a causal relation with increased risk of cardiovascular disease (the so-called lipid hypothesis).[75][76] However, high cholesterol may be caused by many factors. Other indicators, such as high LDL/HDL ratio, have proved to be more predictive.[76] In a study of myocardial infarction in 52 countries, the ApoB/ApoA1 (related to LDL and HDL, respectively) ratio was the strongest predictor of CVD among all risk factors.[77] There are other pathways involving obesity, triglyceride levels, insulin sensitivity, endothelial function, and thrombogenicity, among others, that play a role in CVD, although it seems, in the absence of an adverse blood lipid profile, the other known risk factors have only a weak atherogenic effect.[78] Different saturated fatty acids have differing effects on various lipid levels.[79]
Cancer
The evidence for a relation between saturated fat intake and cancer is significantly weaker, and there does not seem to be a clear medical consensus about it.
- A meta-analysis published in 2003 found a significant positive relationship between saturated fat and breast cancer.[80] However two subsequent reviews have found weak or insignificant relation,[81][82] and noted the prevalence of confounding factors.[81][83]
- Another review found limited evidence for a positive relationship between consuming animal fat and incidence of colorectal cancer.[84]
- Other meta-analyses found evidence for increased risk of ovarian cancer by high consumption of saturated fat.[85]
- Some studies have indicated that serum myristic acid[86][87] and palmitic acid[87] and dietary myristic[88] and palmitic[88] saturated fatty acids and serum palmitic combined with alpha-tocopherol supplementation[86] are associated with increased risk of prostate cancer in a dose-dependent manner. These associations may, however, reflect differences in intake or metabolism of these fatty acids between the precancer cases and controls, rather than being an actual cause.[87]
Bones
Various animal studies have indicated that the intake of saturated fat has a negative effect on the mineral density of bones. One study suggested that men may be particularly vulnerable.[89]
Disposition and overall health
Studies have shown that substituting monounsaturated fatty acids for saturated ones is associated with increased daily physical activity and resting energy expenditure. More physical activity, less anger, and less irritability were associated with a higher-oleic acid diet than one of a palmitic acid diet.[90]
Monounsaturated vs. polyunsaturated fat
The most common fatty acids in human diet are unsaturated or mono-unsaturated. Monounsaturated fats are found in animal flesh such as red meat, whole milk products, nuts, and high fat fruits such as olives and avocados. Olive oil is about 75% monounsaturated fat.[91] The high oleic variety sunflower oil contains at least 70% monounsaturated fat.[92] Canola oil and cashews are both about 58% monounsaturated fat.[93] Tallow (beef fat) is about 50% monounsaturated fat,[94] and lard is about 40% monounsaturated fat.[95] Other sources include hazelnut, avocado oil, macadamia nut oil, grapeseed oil, groundnut oil (peanut oil), sesame oil, corn oil, popcorn, whole grain wheat, cereal, oatmeal, almond oil, hemp oil, and tea-oil camellia.[96]
Polyunsaturated fatty acids can be found mostly in nuts, seeds, fish, seed oils, and oysters.[97]
Food sources of polyunsaturated fats include:[97][98]
| Food source (100g) | Polyunsaturated fat (g) |
|---|---|
| Walnuts | 47 |
| Canola oil | 34 |
| Sunflower seeds | 33 |
| Sesame seeds | 26 |
| Chia seeds | 23.7 |
| Unsalted peanuts | 16 |
| Peanut butter | 14.2 |
| Avocado oil | 13.5[99] |
| Olive oil | 11 |
| Safflower oil | 12.82[100] |
| Seaweed | 11 |
| Sardines | 5 |
| Soybeans | 7 |
| Tuna | 14 |
| Wild salmon | 17.3 |
| Whole grain wheat | 9.7 |
Insulin resistance and sensitivity
MUFAs (especially oleic acid) have been found to lower the incidence of insulin resistance; PUFAs (especially large amounts of arachidonic acid) and SFAs (such as arachidic acid) increased it. These ratios can be indexed in the phospholipids of human skeletal muscle and in other tissues as well. This relationship between dietary fats and insulin resistance is presumed secondary to the relationship between insulin resistance and inflammation, which is partially modulated by dietary fat ratios (omega−3/6/9) with both omega−3 and −9 thought to be anti-inflammatory, and omega−6 pro-inflammatory (as well as by numerous other dietary components, particularly polyphenols and exercise, with both of these anti-inflammatory). Although both pro- and anti-inflammatory types of fat are biologically necessary, fat dietary ratios in most US diets are skewed towards omega−6, with subsequent disinhibition of inflammation and potentiation of insulin resistance.[42] This is contrary to the suggestion that polyunsaturated fats are shown to be protective against insulin resistance.[citation needed]
The large scale KANWU study found that increasing MUFA and decreasing SFA intake could improve insulin sensitivity, but only when the overall fat intake of the diet was low.[101] However, some MUFAs may promote insulin resistance (like the SFAs), whereas PUFAs may protect against it.[102][103][clarification needed]
Cancer
Levels of oleic acid along with other MUFAs in red blood cell membranes were positively associated with breast cancer risk. The saturation index (SI) of the same membranes was inversely associated with breast cancer risk. MUFAs and low SI in erythrocyte membranes are predictors of postmenopausal breast cancer. Both of these variables depend on the activity of the enzyme delta-9 desaturase (Δ9-d).[104]
Results from observational clinical trials on PUFA intake and cancer have been inconsistent and vary by numerous factors of cancer incidence, including gender and genetic risk.[105] Some studies have shown associations between higher intakes and/or blood levels of omega-3 PUFAs and a decreased risk of certain cancers, including breast and colorectal cancer, while other studies found no associations with cancer risk.[105][106]
Pregnancy disorders
Polyunsaturated fat supplementation was found to have no effect on the incidence of pregnancy-related disorders, such as hypertension or preeclampsia, but may increase the length of gestation slightly and decreased the incidence of early premature births.[97]
Expert panels in the United States and Europe recommend that pregnant and lactating women consume higher amounts of polyunsaturated fats than the general population to enhance the DHA status of the fetus and newborn.[97]
"Cis fat" vs. "trans fat"
In nature, unsaturated fatty acids generally have double bonds in cis configuration (with the adjacent C–C bonds on the same side) as opposed to trans.[107] Nevertheless, trans fatty acids (TFAs) occur in small amounts in meat and milk of ruminants (such as cattle and sheep),[108][109] typically 2–5% of total fat.[110] Natural TFAs, which include conjugated linoleic acid (CLA) and vaccenic acid, originate in the rumen of these animals. CLA has two double bonds, one in the cis configuration and one in trans, which makes it simultaneously a cis- and a trans-fatty acid.[111]
| Food type | Trans fat content |
|---|---|
| butter | 2 to 7 g |
| whole milk | 0.07 to 0.1 g |
| animal fat | 0 to 5 g[110] |
| ground beef | 1 g |
Concerns about trans fatty acids in human diet were raised when they were found to be an unintentional byproduct of the partial hydrogenation of vegetable and fish oils. While these trans fatty acids (popularly called "trans fats") are edible, they have been implicated in many health problems.[113]
The hydrogenation process, invented and patented by Wilhelm Normann in 1902, made it possible to turn relatively cheap liquid fats such as whale or fish oil into more solid fats and to extend their shelf-life by preventing rancidification. (The source fat and the process were initially kept secret to avoid consumer distaste.[114]) This process was widely adopted by the food industry in the early 1900s; first for the production of margarine, a replacement for butter and shortening,[115] and eventually for various other fats used in snack food, packaged baked goods, and deep fried products.[116]
Full hydrogenation of a fat or oil produces a fully saturated fat. However, hydrogenation generally was interrupted before completion, to yield a fat product with specific melting point, hardness, and other properties. Partial hydrogenation turns some of the cis double bonds into trans bonds by an isomerization reaction.[116][117] The trans configuration is favored [citation needed] because it is the lower energy form.
This side reaction accounts for most of the trans fatty acids consumed today, by far.[118][119] An analysis of some industrialized foods in 2006 found up to 30% "trans fats" in artificial shortening, 10% in breads and cake products, 8% in cookies and crackers, 4% in salty snacks, 7% in cake frostings and sweets, and 26% in margarine and other processed spreads.[112] Another 2010 analysis however found only 0.2% of trans fats in margarine and other processed spreads.[120] Up to 45% of the total fat in those foods containing man-made trans fats formed by partially hydrogenating plant fats may be trans fat.[110] Baking shortenings, unless reformulated, contain around 30% trans fats compared to their total fats. High-fat dairy products such as butter contain about 4%. Margarines not reformulated to reduce trans fats may contain up to 15% trans fat by weight,[121] but some reformulated ones are less than 1% trans fat.
High levels of TFAs have been recorded in popular "fast food" meals.[119] An analysis of samples of McDonald's French fries collected in 2004 and 2005 found that fries served in New York City contained twice as much trans fat as in Hungary, and 28 times as much as in Denmark , where trans fats are restricted. For Kentucky Fried Chicken products, the pattern was reversed: the Hungarian product containing twice the trans fat of the New York product. Even within the United States, there was variation, with fries in New York containing 30% more trans fat than those from Atlanta.[122]
Cardiovascular disease
Numerous studies have found that consumption of TFAs increases risk of cardiovascular disease.[14][5] The Harvard School of Public Health advises that replacing TFAs and saturated fats with cis monounsaturated and polyunsaturated fats is beneficial for health.[123]
Consuming trans fats has been shown to increase the risk of coronary artery disease in part by raising levels of low-density lipoprotein (LDL, often termed "bad cholesterol"), lowering levels of high-density lipoprotein (HDL, often termed "good cholesterol"), increasing triglycerides in the bloodstream and promoting systemic inflammation.[124][125]
The primary health risk identified for trans fat consumption is an elevated risk of coronary artery disease (CAD).[126] A 1994 study estimated that over 30,000 cardiac deaths per year in the United States are attributable to the consumption of trans fats.[127] By 2006 upper estimates of 100,000 deaths were suggested.[128] A comprehensive review of studies of trans fats published in 2006 in the New England Journal of Medicine reports a strong and reliable connection between trans fat consumption and CAD, concluding that "On a per-calorie basis, trans fats appear to increase the risk of CAD more than any other macronutrient, conferring a substantially increased risk at low levels of consumption (1 to 3% of total energy intake)".[129]
The major evidence for the effect of trans fat on CAD comes from the Nurses' Health Study – a cohort study that has been following 120,000 female nurses since its inception in 1976. In this study, Hu and colleagues analyzed data from 900 coronary events from the study's population during 14 years of followup. He determined that a nurse's CAD risk roughly doubled (relative risk of 1.93, CI: 1.43 to 2.61) for each 2% increase in trans fat calories consumed (instead of carbohydrate calories). By contrast, for each 5% increase in saturated fat calories (instead of carbohydrate calories) there was a 17% increase in risk (relative risk of 1.17, CI: 0.97 to 1.41). "The replacement of saturated fat or trans unsaturated fat by cis (unhydrogenated) unsaturated fats was associated with larger reductions in risk than an isocaloric replacement by carbohydrates."[130] Hu also reports on the benefits of reducing trans fat consumption. Replacing 2% of food energy from trans fat with non-trans unsaturated fats more than halves the risk of CAD (53%). By comparison, replacing a larger 5% of food energy from saturated fat with non-trans unsaturated fats reduces the risk of CAD by 43%.[130]
Another study considered deaths due to CAD, with consumption of trans fats being linked to an increase in mortality, and consumption of polyunsaturated fats being linked to a decrease in mortality.[126][131]
Trans fat has been found to act like saturated in raising the blood level of LDL ("bad cholesterol"); but, unlike saturated fat, it also decreases levels of HDL ("good cholesterol"). The net increase in LDL/HDL ratio with trans fat, a widely accepted indicator of risk for coronary artery disease, is approximately double that due to saturated fat.[132][133][134] One randomized crossover study published in 2003 comparing the effect of eating a meal on blood lipids of (relatively) cis and trans-fat-rich meals showed that cholesteryl ester transfer (CET) was 28% higher after the trans meal than after the cis meal and that lipoprotein concentrations were enriched in apolipoprotein(a) after the trans meals.[135]
The citokyne test is a potentially more reliable indicator of CAD risk, although is still being studied.[126] A study of over 700 nurses showed that those in the highest quartile of trans fat consumption had blood levels of C-reactive protein (CRP) that were 73% higher than those in the lowest quartile.[136]
Breast feeding
It has been established that trans fats in human breast milk fluctuate with maternal consumption of trans fat, and that the amount of trans fats in the bloodstream of breastfed infants fluctuates with the amounts found in their milk. In 1999, reported percentages of trans fats (compared to total fats) in human milk ranged from 1% in Spain, 2% in France, 4% in Germany, and 7% in Canada and the United States.[137]
Other health risks
There are suggestions that the negative consequences of trans fat consumption go beyond the cardiovascular risk. In general, there is much less scientific consensus asserting that eating trans fat specifically increases the risk of other chronic health problems:
- Alzheimer's disease: A study published in Archives of Neurology in February 2003 suggested that the intake of both trans fats and saturated fats promotes the development of Alzheimer disease,[138] although not confirmed in an animal model.[139] It has been found that trans fats impaired memory and learning in middle-age rats. The brains of rats that ate trans-fats had fewer proteins critical to healthy neurological function. Inflammation in and around the hippocampus, the part of the brain responsible for learning and memory. These are the exact types of changes normally seen at the onset of Alzheimer's, but seen after six weeks, even though the rats were still young.[140]
- Cancer: There is no scientific consensus that consuming trans fats significantly increases cancer risks across the board.[126] The American Cancer Society states that a relationship between trans fats and cancer "has not been determined."[141] One study has found a positive connection between trans fat and prostate cancer.[142] However, a larger study found a correlation between trans fats and a significant decrease in high-grade prostate cancer.[143] An increased intake of trans fatty acids may raise the risk of breast cancer by 75%, suggest the results from the French part of the European Prospective Investigation into Cancer and Nutrition.[144][145]
- Diabetes: There is a growing concern that the risk of type 2 diabetes increases with trans fat consumption.[126][146] However, consensus has not been reached.[129] For example, one study found that risk is higher for those in the highest quartile of trans fat consumption.[147] Another study has found no diabetes risk once other factors such as total fat intake and BMI were accounted for.[148]
- Obesity: Research indicates that trans fat may increase weight gain and abdominal fat, despite a similar caloric intake.[149] A 6-year experiment revealed that monkeys fed a trans fat diet gained 7.2% of their body weight, as compared to 1.8% for monkeys on a mono-unsaturated fat diet.[150][151] Although obesity is frequently linked to trans fat in the popular media,[152] this is generally in the context of eating too many calories; there is not a strong scientific consensus connecting trans fat and obesity, although the 6-year experiment did find such a link, concluding that "under controlled feeding conditions, long-term TFA consumption was an independent factor in weight gain. TFAs enhanced intra-abdominal deposition of fat, even in the absence of caloric excess, and were associated with insulin resistance, with evidence that there is impaired post-insulin receptor binding signal transduction."[151]
- Infertility in women: One 2007 study found, "Each 2% increase in the intake of energy from trans unsaturated fats, as opposed to that from carbohydrates, was associated with a 73% greater risk of ovulatory infertility...".[153]
- Major depressive disorder: Spanish researchers analysed the diets of 12,059 people over six years and found that those who ate the most trans fats had a 48 per cent higher risk of depression than those who did not eat trans fats.[154] One mechanism may be trans-fats' substitution for docosahexaenoic acid (DHA) levels in the orbitofrontal cortex (OFC). Very high intake of trans-fatty acids (43% of total fat) in mice from 2 to 16 months of age was associated with lowered DHA levels in the brain (p=0.001).[139] When the brains of 15 major depressive subjects who had committed suicide were examined post-mortem and compared against 27 age-matched controls, the suicidal brains were found to have 16% less (male average) to 32% less (female average) DHA in the OFC. The OFC controls reward, reward expectation, and empathy (all of which are reduced in depressive mood disorders) and regulates the limbic system.[155]
- Behavioral irritability and aggression: a 2012 observational analysis of subjects of an earlier study found a strong relation between dietary trans fat acids and self-reported behavioral aggression and irritability, suggesting but not establishing causality.[156]
- Diminished memory: In a 2015 article, researchers re-analyzing results from the 1999-2005 UCSD Statin Study argue that "greater dietary trans fatty acid consumption is linked to worse word memory in adults during years of high productivity, adults age <45".[157]
- Acne: According to a 2015 study, trans fats are one of several components of Western pattern diets which promote acne, along with carbohydrates with high glycemic load such as refined sugars or refined starches, milk and dairy products, and saturated fats, while omega-3 fatty acids, which reduce acne, are deficient in Western pattern diets.[158]
Biochemical mechanisms
The exact biochemical process by which trans fats produce specific health problems are a topic of continuing research. Intake of dietary trans fat perturbs the body's ability to metabolize essential fatty acids (EFAs, including omega-3) leading to changes in the phospholipid fatty acid composition of the arterial walls, thereby raising risk of coronary artery disease.[159]
Trans double bonds are claimed to induce a linear conformation to the molecule, favoring its rigid packing as in plaque formation. The geometry of the cis double bond, in contrast, is claimed to create a bend in the molecule, thereby precluding rigid formations.[160]
While the mechanisms through which trans fatty acids contribute to coronary artery disease are fairly well understood, the mechanism for their effects on diabetes is still under investigation. They may impair the metabolism of long-chain polyunsaturated fatty acids (LCPUFAs).[161] However, maternal pregnancy trans fatty acid intake has been inversely associated with LCPUFAs levels in infants at birth thought to underlie the positive association between breastfeeding and intelligence.[162]
Trans fats are processed by the liver differently than other fats. They may cause liver dysfunction by interfering with delta 6 desaturase, an enzyme involved in converting essential fatty acids to arachidonic acid and prostaglandins, both of which are important to the functioning of cells.[163]
Natural "trans fats" in dairy products
Some trans fatty acids occur in natural fats and traditionally processed foods. Vaccenic acid occurs in breast milk, and some isomers of conjugated linoleic acid (CLA) are found in meat and dairy products from ruminants. Butter, for example, contains about 3% trans fat.[164]
The U.S. National Dairy Council has asserted that the trans fats present in animal foods are of a different type than those in partially hydrogenated oils, and do not appear to exhibit the same negative effects.[165] A review agrees with the conclusion (stating that "the sum of the current evidence suggests that the Public health implications of consuming trans fats from ruminant products are relatively limited") but cautions that this may be due to the low consumption of trans fats from animal sources compared to artificial ones.[129]
In 2008 a meta-analysis found that all trans fats, regardless of natural or artificial origin equally raise LDL and lower HDL levels.[166] Other studies though have shown different results when it comes to animal-based trans fats like conjugated linoleic acid (CLA). Although CLA is known for its anticancer properties, researchers have also found that the cis-9, trans-11 form of CLA can reduce the risk for cardiovascular disease and help fight inflammation.[167][168]
Two Canadian studies have shown that vaccenic acid, a TFA that naturally occurs in dairy products, could be beneficial compared to hydrogenated vegetable shortening, or a mixture of pork lard and soy fat, by lowering total LDL and triglyceride levels.[169][170][171] A study by the US Department of Agriculture showed that vaccenic acid raises both HDL and LDL cholesterol, whereas industrial trans fats only raise LDL with no beneficial effect on HDL.[172]
Official recommendations
In light of recognized evidence and scientific agreement, nutritional authorities consider all trans fats equally harmful for health and recommend that their consumption be reduced to trace amounts.[173][174][175][176][177] In 2003, the WHO recommended that trans fats make up no more than 0.9% of a person's diet[110] and, in 2018, introduced a 6-step guide to eliminate industrially-produced trans-fatty acids from the global food supply.[178]
The National Academy of Sciences (NAS) advises the U.S. and Canadian governments on nutritional science for use in public policy and product labeling programs. Their 2002 Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids[179] contains their findings and recommendations regarding consumption of trans fat.[180]
Their recommendations are based on two key facts. First, "trans fatty acids are not essential and provide no known benefit to human health",[124] whether of animal or plant origin.[181] Second, given their documented effects on the LDL/HDL ratio,[125] the NAS concluded "that dietary trans fatty acids are more deleterious with respect to coronary artery disease than saturated fatty acids". A 2006 review published in the New England Journal of Medicine (NEJM) that states "from a nutritional standpoint, the consumption of trans fatty acids results in considerable potential harm but no apparent benefit."[129]
Because of these facts and concerns, the NAS has concluded there is no safe level of trans fat consumption. There is no adequate level, recommended daily amount or tolerable upper limit for trans fats. This is because any incremental increase in trans fat intake increases the risk of coronary artery disease.[125]
Despite this concern, the NAS dietary recommendations have not included eliminating trans fat from the diet. This is because trans fat is naturally present in many animal foods in trace quantities, and thus its removal from ordinary diets might introduce undesirable side effects and nutritional imbalances. The NAS has, thus, "recommended that trans fatty acid consumption be as low as possible while consuming a nutritionally adequate diet".[182] Like the NAS, the WHO has tried to balance public health goals with a practical level of trans fat consumption, recommending in 2003 that trans fats be limited to less than 1% of overall energy intake.[110]
Regulatory action
In the last few decades, there has been substantial amount of regulation in many countries, limiting trans fat contents of industrialized and commercial food products.
Alternatives to hydrogenation
The negative public image and strict regulations has led to interest in replacing partial hydrogenation. In fat interesterification, the fatty acids are among a mix of triglycerides. When applied to a suitable blend of oils and saturated fats, possibly followed by separation of unwanted solid or liquid triglycerides, this process could conceivably achieve results similar to those of partial hydrogenation without affecting the fatty acids themselves; in particular, without creating any new "trans fat".
Hydrogenation can be achieved with only small production of trans fat. The high-pressure methods produced margarine containing 5 to 6% trans fat. Based on current U.S. labeling requirements (see below), the manufacturer could claim the product was free of trans fat.[183] The level of trans fat may also be altered by modification of the temperature and the length of time during hydrogenation.
One can mix oils (such as olive, soybean, and canola), water, monoglycerides, and fatty acids to form a "cooking fat" that acts the same way as trans and saturated fats.[184][185]
Omega-three and omega-six fatty acids
The ω−3 fatty acids have received substantial attention. Among omega-3 fatty acids, neither long-chain nor short-chain forms were consistently associated with breast cancer risk. High levels of docosahexaenoic acid (DHA), however, the most abundant omega-3 polyunsaturated fatty acid in erythrocyte (red blood cell) membranes, were associated with a reduced risk of breast cancer.[104] The DHA obtained through the consumption of polyunsaturated fatty acids is positively associated with cognitive and behavioral performance.[186] In addition, DHA is vital for the grey matter structure of the human brain, as well as retinal stimulation and neurotransmission.[97]
Interesterification
Some studies have investigated the health effects of interesterified (IE) fats, by comparing diets with IE and non-IE fats with the same overall fatty acid composition.[187]
Several experimental studies in humans found no statistical difference on fasting blood lipids between a diet with large amounts of IE fat, having 25-40% C16:0 or C18:0 on the 2-position, and a similar diet with non-IE fat, having only 3-9% C16:0 or C18:0 on the 2-position.[188][189][190] A negative result was obtained also in a study that compared the effects on blood cholesterol levels of an IE fat product mimicking cocoa butter and the real non-IE product.[191][192][193][194][195][196][197]
A 2007 study funded by the Malaysian Palm Oil Board[198] claimed that replacing natural palm oil by other interesterified or partially hydrogenated fats caused adverse health effects, such as higher LDL/HDL ratio and plasma glucose levels. However, these effects could be attributed to the higher percentage of saturated acids in the IE and partially hydrogenated fats, rather than to the IE process itself.[199][200]
Role in disease
In the human body, high levels of triglycerides in the bloodstream have been linked to atherosclerosis, heart disease[201] and stroke.[9] However, the relative negative impact of raised levels of triglycerides compared to that of LDL:HDL ratios is as yet unknown. The risk can be partly accounted for by a strong inverse relationship between triglyceride level and HDL-cholesterol level. But the risk is also due to high triglyceride levels increasing the quantity of small, dense LDL particles.[202]
Guidelines
The National Cholesterol Education Program has set guidelines for triglyceride levels:[203][204]
| Level | Interpretation | |
|---|---|---|
| (mg/dL) | (mmol/L) | |
| < 150 | < 1.70 | Normal range – low risk |
| 150–199 | 1.70–2.25 | Slightly above normal |
| 200–499 | 2.26–5.65 | Some risk |
| 500 or higher | > 5.65 | Very high – high risk |
These levels are tested after fasting 8 to 12 hours. Triglyceride levels remain temporarily higher for a period after eating.
The AHA recommends an optimal triglyceride level of 100 mg/dL (1.1 mmol/L) or lower to improve heart health.[205]
Reducing triglyceride levels
Weight loss and dietary modification are effective first-line lifestyle modification treatments for hypertriglyceridemia.[206] For people with mildly or moderately high levels of triglycerides, lifestyle changes, including weight loss, moderate exercise[207][208] and dietary modification, are recommended.[209] This may include restriction of carbohydrates (specifically fructose)[206] and fat in the diet and the consumption of omega-3 fatty acids[208] from algae, nuts, fish and seeds.[210] Medications are recommended in those with high levels of triglycerides that are not corrected with the aforementioned lifestyle modifications, with fibrates being recommended first.[209][211][212] Omega-3-carboxylic acids is another prescription drug used to treat very high levels of blood triglycerides.[213]
The decision to treat hypertriglyceridemia with medication depends on the levels and on the presence of other risk factors for cardiovascular disease. Very high levels that would increase the risk of pancreatitis are treated with a drug from the fibrate class. Niacin and omega-3 fatty acids as well as drugs from the statin class may be used in conjunction, with statins being the main medication for moderate hypertriglyceridemia when reduction of cardiovascular risk is required.[209]
Fat digestion and metabolism
Fats are broken down in the healthy body to release their constituents, glycerol and fatty acids. Glycerol itself can be converted to glucose by the liver and so become a source of energy. Fats and other lipids are broken down in the body by enzymes called lipases produced in the pancreas.
Many cell types can use either glucose or fatty acids as a source of energy for metabolism. In particular, heart and skeletal muscle prefer fatty acids.[citation needed] Despite long-standing assertions to the contrary, fatty acids can also be used as a source of fuel for brain cells through mitochondrial oxidation.[214]
See also
- Animal fat
- Monounsaturated fat
- Diet and heart disease
- Fatty acid synthesis
- Food composition data
- Western pattern diet
- Oil
- Lipid
References
- ↑ 1.0 1.1 1.2 1.3 Entry for "fat" in the online Merriam-Webster disctionary, sense 3.2. Accessed on 2020-08-09
- ↑ 2.0 2.1 2.2 Thomas A. B. Sanders (2016): "The Role of Fats in Human Diet". Pages 1-20 of Functional Dietary Lipids. Woodhead/Elsevier, 332 pages. ISBN 978-1-78242-247-1doi: 10.1016/B978-1-78242-247-1.00001-6
- ↑ "Macronutrients: the Importance of Carbohydrate, Protein, and Fat". University of Illinois at Urbana–Champaign. http://www.mckinley.illinois.edu/handouts/macronutrients.htm.
- ↑ "Introduction to Energy Storage". Khan Academy. http://www.khanacademy.org/test-prep/mcat/biomolecules/fat-and-protein-metabolism/v/introduction-to-energy-storage.
- ↑ 5.0 5.1 5.2 Government of the United Kingdom (1996): "Schedule 7: Nutrition labelling ". In Food Labelling Regulations 1996 . Accessed on 2020-08-09.
- ↑ Wu, Yang; Zhang, Aijun; Hamilton, Dale J.; Deng, Tuo (2017). "Epicardial Fat in the Maintenance of Cardiovascular Health". Methodist DeBakey Cardiovascular Journal 13 (1): 20–24. doi:10.14797/mdcj-13-1-20. ISSN 1947-6094. PMID 28413578.
- ↑ "The human proteome in adipose - The Human Protein Atlas". http://www.proteinatlas.org/humanproteome/adipose.
- ↑ White, Hayden; Venkatesh, Balasubramanian (2011). "Clinical review: Ketones and brain injury". Critical Care 15 (2): 219. doi:10.1186/cc10020. PMID 21489321.
- ↑ 9.0 9.1 Drummond, K. E.; Brefere, L. M. (2014). Nutrition for Foodservice and Culinary Professionals (8th ed.). John Wiley & Sons. ISBN 978-0-470-05242-6.
- ↑ Rebecca J. Donatelle (2005): Health, the Basics, 6th edition. Pearson Education, San Francisco; ISBN 978-0-13-120687-8
- ↑ Frank B. Hu, JoAnn E. Manson, and Walter C. Willett (2001): "Types of dietary fat and risk of coronary heart disease: A critical review". Journal of the American College of Nutrition, volume 20, issue 1, pages 5-19. doi: 10.1080/07315724.2001.10719008
- ↑ Lee Hooper, Carolyn D. Summerbell, Julian P. T. Higgins, Rachel L. Thompson, Nigel E. Capps, George Davey Smith, Rudolph A. Riemersma, and Shah Ebrahim (2001): "Dietary fat intake and prevention of cardiovascular disease: systematic review". The BMJ, volume 322, pages 757-. doi: 10.1136/bmj.322.7289.757
- ↑ George A. Bray, Sahasporn Paeratakul, Barry M. Popkin (2004): "Dietary fat and obesity: a review of animal, clinical and epidemiological studies". Physiology & Behavior, volume 83, issue 4, pages 549-555. doi: 10.1016/j.physbeh.2004.08.039
- ↑ 14.0 14.1 Dariush Mozaffarian, Martijn B. Katan, Alberto Ascherio, Meir J. Stampfer, and Walter C. Willett (2006): "Trans fatty acids and cardiovascular disease". New England Journal of Medicine, volume 354, issue 15, pages 1601–1613. doi: 10.1056/NEJMra054035 PMID 16611951
- ↑ "Saturated fats". American Heart Association. 2014. http://www.heart.org/HEARTORG/GettingHealthy/FatsAndOils/Fats101/Saturated-Fats_UCM_301110_Article.jsp.
- ↑ "Top food sources of saturated fat in the US". Harvard University School of Public Health. 2014. http://www.hsph.harvard.edu/nutritionsource/top-food-sources-of-saturated-fat-in-the-us/.
- ↑ "Saturated, Unsaturated, and Trans Fats". choosemyplate.gov. 2020. https://www.choosemyplate.gov/node/5664.
- ↑ Reece, Jane; Campbell, Neil (2002). Biology. San Francisco: Benjamin Cummings. pp. 69–70. ISBN 978-0-8053-6624-2. https://archive.org/details/biologyc00camp/page/69.
- ↑ "What are "oils"?". ChooseMyPlate.gov, US Department of Agriculture. 2015. http://www.choosemyplate.gov/food-groups/oils.html.
- ↑ "Reduction in saturated fat intake for cardiovascular disease". The Cochrane Database of Systematic Reviews 6 (6): CD011737. June 2015. doi:10.1002/14651858.CD011737. PMID 26068959.
- ↑ Hooper, L; Martin, N; Jimoh, OF; Kirk, C; Foster, E; Abdelhamid, AS (21 August 2020). "Reduction in saturated fat intake for cardiovascular disease.". The Cochrane Database of Systematic Reviews 2020 (8): CD011737. doi:10.1002/14651858.CD011737.pub3. PMID 32827219.
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 "Dietary Fats and Cardiovascular Disease: A Presidential Advisory From the American Heart Association". Circulation 136 (3): e1–e23. July 2017. doi:10.1161/CIR.0000000000000510. PMID 28620111.
- ↑ "Healthy diet Fact sheet N°394". May 2015. https://www.who.int/mediacentre/factsheets/fs394/en/.
- ↑ World Health Organization: Food pyramid (nutrition)
- ↑ "Fats explained". https://www.heartuk.org.uk/downloads/factsheets/fats-explained.pdf.
- ↑ "Live Well, Eat well, Fat: the facts". 27 April 2018. https://www.nhs.uk/live-well/eat-well/different-fats-nutrition/.
- ↑ "Fat: the facts". United Kingdom's National Health Service. 2018-04-27. https://www.nhs.uk/live-well/eat-well/different-fats-nutrition/.
- ↑ "How to eat less saturated fat - NHS". April 27, 2018. https://www.nhs.uk/live-well/eat-well/eat-less-saturated-fat/.
- ↑ "Fats explained - types of fat | BHF". https://www.bhf.org.uk/heart-health/preventing-heart-disease/healthy-eating/fats-explained.
- ↑ "Key Recommendations: Components of Healthy Eating Patterns". https://health.gov/dietaryguidelines/2015/guidelines/chapter-1/key-recommendations/.
- ↑ "Cut Down on Saturated Fats". United States Department of Health and Human Services. https://health.gov/dietaryguidelines/2015/resources/DGA_Cut-Down-On-Saturated-Fats.pdf.
- ↑ "Trends in Intake of Energy, Protein, Carbohydrate, Fat, and Saturated Fat — United States, 1971–2000". Centers for Disease Control. 2004. https://www.cdc.gov/od/oc/media/mmwrnews/n040206.htm#mmwr2.
- ↑ "Dietary Guidelines for Americans". United States Department of Agriculture. 2005. https://www.fda.gov/ohrms/dockets/dockets/06q0458/06q-0458-sup0001-02.pdf.
- ↑ "Dietary Guidelines for Indians - A Manual". http://ninindia.org/DietaryGuidelinesforNINwebsite.pdf.
- ↑ "Health Diet". India's Ministry of Health and Family Welfare. https://www.nhp.gov.in/healthlyliving/healthy-diet.
- ↑ "Choosing foods with healthy fats". Health Canada. 2018-10-10. https://food-guide.canada.ca/en/healthy-eating-recommendations/make-it-a-habit-to-eat-vegetables-fruit-whole-grains-and-protein-foods/choosing-foods-with-healthy-fats/.
- ↑ "Fat". Australia's National Health and Medical Research Council and Department of Health and Ageing. 2012-09-24. https://www.eatforhealth.gov.au/food-essentials/fat-salt-sugars-and-alcohol/fat.
- ↑ "Getting the Fats Right!". Singapore's Ministry of Health. https://www.healthhub.sg/live-healthy/458/Getting%20the%20Fats%20Right.
- ↑ "Eating and Activity Guidelines for New Zealand Adults". New Zealand's Ministry of Health. https://www.health.govt.nz/system/files/documents/publications/eating-activity-guidelines-for-new-zealand-adults-oct15_0.pdf.
- ↑ "Know More about Fat". Hong Kong's Department of Health. https://www.chp.gov.hk/en/static/100023.html.
- ↑ "Saturated fats: what dietary intake?". American Journal of Clinical Nutrition 80 (3): 550–559. September 2004. doi:10.1093/ajcn/80.3.550. PMID 15321792.
- ↑ 42.0 42.1 "Dietary fats and insulin action". Diabetologia 39 (6): 621–31. June 1996. doi:10.1007/BF00418533. PMID 8781757.
- ↑ 43.0 43.1 43.2 43.3 Joint WHO/FAO Expert Consultation (2003). Diet, Nutrition and the Prevention of Chronic Diseases (WHO technical report series 916). World Health Organization. pp. 81–94. ISBN 978-92-4-120916-8. http://apps.who.int/iris/bitstream/10665/42665/1/WHO_TRS_916.pdf. Retrieved 2016-04-04.
- ↑ Zelman K (2011). "The Great Fat Debate: A Closer Look at the Controversy—Questioning the Validity of Age-Old Dietary Guidance". Journal of the American Dietetic Association 111 (5): 655–658. doi:10.1016/j.jada.2011.03.026. PMID 21515106.
- ↑ Nutrition, Center for Food Safety and Applied (2022-03-07). "Health Claim Notification for Saturated Fat, Cholesterol, and Trans Fat, and Reduced Risk of Heart Disease" (in en). FDA. https://www.fda.gov/food/food-labeling-nutrition/health-claim-notification-saturated-fat-cholesterol-and-trans-fat-and-reduced-risk-heart-disease.
- ↑ "Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee". Circulation 114 (1): 82–96. July 2006. doi:10.1161/CIRCULATIONAHA.106.176158. PMID 16785338.
- ↑ "Principles for national and regional guidelines on cardiovascular disease prevention: a scientific statement from the World Heart and Stroke Forum". Circulation 109 (25): 3112–21. June 2004. doi:10.1161/01.CIR.0000133427.35111.67. PMID 15226228. http://www.sisalombardia.it/pdfs/guideline_world_heart_and_stroke_forum.pdf.
- ↑ "Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials". European Journal of Clinical Nutrition 72 (1): 30–43. January 2018. doi:10.1038/ejcn.2017.58. PMID 28488692.
- ↑ "Mediterranean diet and health outcomes: a systematic meta-review". European Journal of Public Health 28 (5): 955–961. October 2018. doi:10.1093/eurpub/cky113. PMID 29992229.
- ↑ "Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis". BMJ 346: e8707. February 2013. doi:10.1136/bmj.e8707. PMID 23386268.
- ↑ Interview: Walter Willett (2017). "Research Review: Old data on dietary fats in context with current recommendations: Comments on Ramsden et al. in the British Medical Journal". TH Chan School of Public Health, Harvard University, Boston. https://www.hsph.harvard.edu/nutritionsource/2016/04/13/diet-heart-ramsden-mce-bmj-comments/.
- ↑ "Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies". BMJ 351 (Aug 11): h3978. August 2015. doi:10.1136/bmj.h3978. PMID 26268692.
- ↑ "Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis". BMJ 346: e8707. February 2013. doi:10.1136/bmj.e8707. PMID 23386268.
- ↑ "Re-evaluation of the traditional diet-heart hypothesis: analysis of recovered data from Minnesota Coronary Experiment (1968-73)". BMJ 353: i1246. April 2016. doi:10.1136/bmj.i1246. PMID 27071971.
- ↑ "Omega-3 Polyunsaturated Fatty Acids: The Way Forward in Times of Mixed Evidence". BioMed Research International 2015: 143109. 2015. doi:10.1155/2015/143109. PMID 26301240.
- ↑ 56.0 56.1 "Reduction in saturated fat intake for cardiovascular disease". Cochrane Database of Systematic Reviews 5 (5): CD011737. 2020. doi:10.1002/14651858.CD011737.pub2. ISSN 1465-1858. PMID 32428300.
- ↑ "European guidelines on cardiovascular disease prevention in clinical practice: executive summary". European Heart Journal 28 (19): 2375–2414. 2007. doi:10.1093/eurheartj/ehm316. PMID 17726041.
- ↑ Labarthe, Darwin (2011). "Chapter 17 What Causes Cardiovascular Diseases?". Epidemiology and prevention of cardiovascular disease: a global challenge (2nd ed.). Jones and Bartlett Publishers. ISBN 978-0-7637-4689-6.
- ↑ "Position of the American Dietetic Association and Dietitians of Canada: Dietary Fatty Acids". Journal of the American Dietetic Association 107 (9): 1599–1611 [1603]. September 2007. doi:10.1016/j.jada.2007.07.024. PMID 17936958.
- ↑ "Food Fact Sheet - Cholesterol". British Dietetic Association. http://www.bda.uk.com/foodfacts/cholesterol.pdf.
- ↑ 61.0 61.1 "Cardiovascular Disease Risk Factors". World Heart Federation. 30 May 2017. http://www.world-heart-federation.org/cardiovascular-health/cardiovascular-disease-risk-factors.
- ↑ "Lower your cholesterol". National Health Service. http://www.nhs.uk/livewell/healthyhearts/pages/cholesterol.aspx.
- ↑ "Nutrition Facts at a Glance - Nutrients: Saturated Fat". Food and Drug Administration. 2009-12-22. https://www.fda.gov/Food/LabelingNutrition/ConsumerInformation/ucm192658.htm.
- ↑ "Scientific Opinion on Dietary Reference Values for fats, including saturated fatty acids, polyunsaturated fatty acids, monounsaturated fatty acids, trans fatty acids, and cholesterol". European Food Safety Authority. 2010-03-25. http://www.efsa.europa.eu/en/efsajournal/pub/1461.
- ↑ Faculty of Public Health of the Royal Colleges of Physicians of the United Kingdom. "Position Statement on Fat". http://www.fph.org.uk/uploads/ps_fat.pdf.
- ↑ Report of a Joint WHO/FAO Expert Consultation (2003). "Diet, Nutrition and the Prevention of Chronic Diseases". World Health Organization. https://www.who.int/hpr/NPH/docs/who_fao_expert_report.pdf.
- ↑ "Cholesterol". Irish Heart Foundation. http://www.irishheart.ie/iopen24/cholesterol-t-7_20_87.html.
- ↑ U.S. Department of Agriculture and U.S. Department of Health and Human Services (December 2010). Dietary Guidelines for Americans, 2010 (7th ed.). Washington, DC: U.S. Government Printing Office. https://health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf.
- ↑ Cannon, Christopher; O'Gara, Patrick (2007). Critical Pathways in Cardiovascular Medicine (2nd ed.). Lippincott Williams & Wilkins. p. 243.
- ↑ "ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS)". Atherosclerosis 217 Suppl 1 (14): S1-44. July 2011. doi:10.1016/j.atherosclerosis.2011.06.012. PMID 21723445.
- ↑ "Monounsaturated Fat". American Heart Association. https://healthyforgood.heart.org/Eat-smart/Articles/Monounsaturated-Fats.
- ↑ "You Can Control Your Cholesterol: A Guide to Low-Cholesterol Living". MerckSource. http://www.mercksource.com/pp/us/cns/cns_krames_template.jspzQzpgzEzzSzppdocszSzuszSzcnszSzcontentzSzkrameszSz1292_01zPzhtm.
- ↑ "A cross-sectional study of dietary habits and lipid profiles. The Rivas-Vaciamadrid study". European Journal of Pediatrics 167 (2): 149–54. February 2008. doi:10.1007/s00431-007-0439-6. PMID 17333272.
- ↑ "Dietary lipids and blood cholesterol: quantitative meta-analysis of metabolic ward studies". BMJ (Clinical Research Ed.) 314 (7074): 112–7. 1997. doi:10.1136/bmj.314.7074.112. PMID 9006469.
- ↑ "Systematic review on the risk and benefit of different cholesterol-lowering interventions". Arteriosclerosis, Thrombosis, and Vascular Biology 19 (2): 187–195. February 1999. doi:10.1161/01.atv.19.2.187. PMID 9974397.
- ↑ 76.0 76.1 "Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths". Lancet 370 (9602): 1829–39. December 2007. doi:10.1016/S0140-6736(07)61778-4. PMID 18061058.
- ↑ Labarthe, Darwin (2011). "Chapter 11 Adverse Blood Lipid Profile". Epidemiology and prevention of cardiovascular disease: a global challenge (2 ed.). Jones and Bartlett Publishers. p. 290. ISBN 978-0-7637-4689-6.
- ↑ Labarthe, Darwin (2011). "Chapter 11 Adverse Blood Lipid Profile". Epidemiology and prevention of cardiovascular disease: a global challenge (2nd ed.). Jones and Bartlett Publishers. p. 277. ISBN 978-0-7637-4689-6.
- ↑ "Fatty acids and atherosclerotic risk". Atherosclerosis: Diet and Drugs. Handbook of Experimental Pharmacology. 170. Springer. 2005. pp. 165–94. doi:10.1007/3-540-27661-0_5. ISBN 978-3-540-22569-0.
- ↑ "Dietary fat and breast cancer risk revisited: a meta-analysis of the published literature". British Journal of Cancer 89 (9): 1672–1685. November 2003. doi:10.1038/sj.bjc.6601314. PMID 14583769.
- ↑ 81.0 81.1 "Nutrition and primary prevention of breast cancer: foods, nutrients and breast cancer risk.". European Journal of Obstetrics, Gynecology, and Reproductive Biology 123 (2): 139–149. 2005-12-01. doi:10.1016/j.ejogrb.2005.05.011. PMID 16316809.
- ↑ "Impact of diet on breast cancer risk.". Current Opinion in Obstetrics and Gynecology 21 (1): 80–85. February 2009. doi:10.1097/GCO.0b013e32831d7f22. PMID 19125007.
- ↑ "Methods of Epidemiology: Evaluating the Fat–Breast Cancer Hypothesis – Comparing Dietary Instruments and Other Developments". Cancer Journal (Sudbury, Mass.) 14 (2): 69–74. Mar–Apr 2008. doi:10.1097/PPO.0b013e31816a5e02. PMID 18391610.
- ↑ Lin OS (2009). "Acquired risk factors for colorectal cancer". Cancer Epidemiology. Methods in Molecular Biology. 472. pp. 361–72. doi:10.1007/978-1-60327-492-0_16. ISBN 978-1-60327-491-3.
- ↑ "Dietary fat intake and risk of epithelial ovarian cancer: a meta-analysis of 6,689 subjects from 8 observational studies". Nutrition and Cancer 40 (2): 87–91. 2001. doi:10.1207/S15327914NC402_2. PMID 11962260.
- ↑ 86.0 86.1 "Fatty acids and risk of prostate cancer in a nested case-control study in male smokers". Cancer Epidemiology, Biomarkers & Prevention 12 (12): 1422–8. December 2003. PMID 14693732. http://cebp.aacrjournals.org/cgi/pmidlookup?view=long&pmid=14693732.
- ↑ 87.0 87.1 87.2 "Fatty acid composition of plasma phospholipids and risk of prostate cancer in a case-control analysis nested within the European Prospective Investigation into Cancer and Nutrition". The American Journal of Clinical Nutrition 88 (5): 1353–63. November 2008. doi:10.3945/ajcn.2008.26369. PMID 18996872.
- ↑ 88.0 88.1 "Dairy product, saturated fatty acid, and calcium intake and prostate cancer in a prospective cohort of Japanese men". Cancer Epidemiology, Biomarkers & Prevention 17 (4): 930–7. April 2008. doi:10.1158/1055-9965.EPI-07-2681. PMID 18398033.
- ↑ "Dietary saturated fat intake is inversely associated with bone density in humans: Analysis of NHANES III". The Journal of Nutrition 136 (1): 159–165. 2006. doi:10.1093/jn/136.1.159. PMID 16365076.
- ↑ "Substituting dietary monounsaturated fat for saturated fat is associated with increased daily physical activity and resting energy expenditure and with changes in mood". The American Journal of Clinical Nutrition 97 (4): 689–97. April 2013. doi:10.3945/ajcn.112.051730. PMID 23446891.
- ↑ "Health benefits and evaluation of healthcare cost savings if oils rich in monounsaturated fatty acids were substituted for conventional dietary oils in the United States". Nutrition Reviews 75 (3): 163–174. February 2017. doi:10.1093/nutrit/nuw062. PMID 28158733.
- ↑ "A systematic review of high-oleic vegetable oil substitutions for other fats and oils on cardiovascular disease risk factors: implications for novel high-oleic soybean oils". Advances in Nutrition 6 (6): 674–93. November 2015. doi:10.3945/an.115.008979. PMID 26567193.
- ↑ Shute, Nancy (2012-05-02). "Lard Is Back In The Larder, But Hold The Health Claims" (in en). NPR. https://www.npr.org/sections/thesalt/2012/05/02/151868208/lard-is-back-in-the-larder-but-hold-the-health-claims.
- ↑ National Research Council (US) Board on Agriculture and Renewable Resources (1976). Fat content and composition of animal products: proceedings of a symposium, Washington, D.C., December 12-13, 1974. Washington: National Academy of Sciences. ISBN 978-0-309-02440-2. https://www.ncbi.nlm.nih.gov/books/NBK216535/.
- ↑ "Ask the Expert: Concerns about canola oil" (in en-us). 2015-04-13. https://www.hsph.harvard.edu/nutritionsource/2015/04/13/ask-the-expert-concerns-about-canola-oil/.
- ↑ "Optimization of supercritical fluid consecutive extractions of fatty acids and polyphenols from Vitis vinifera grape wastes". Journal of Food Science 80 (1): E101-7. January 2015. doi:10.1111/1750-3841.12715. PMID 25471637.
- ↑ 97.0 97.1 97.2 97.3 97.4 "Essential Fatty Acids". Micronutrient Information Center, Oregon State University, Corvallis, OR. May 2014. http://lpi.oregonstate.edu/mic/other-nutrients/essential-fatty-acids.
- ↑ "National nutrient database for standard reference, release 23". United States Department of Agriculture, Agricultural Research Service. 2011. http://www.nal.usda.gov/fnic/foodcomp/search/.
- ↑ "Vegetable oil, avocado Nutrition Facts & Calories". http://nutritiondata.self.com/facts/fats-and-oils/620/2.
- ↑ "United States Department of Agriculture – National Nutrient Database". 8 September 2015. http://ndb.nal.usda.gov/ndb/foods/show/658?manu=&fgcd=.
- ↑ "Substituting dietary saturated for monounsaturated fat impairs insulin sensitivity in healthy men and women: The KANWU Study". Diabetologia 44 (3): 312–9. March 2001. doi:10.1007/s001250051620. PMID 11317662.
- ↑ "The influence of dietary fat on insulin resistance". Current Diabetes Reports 2 (5): 435–40. October 2002. doi:10.1007/s11892-002-0098-y. PMID 12643169.
- ↑ "Role of fatty acid composition in the development of metabolic disorders in sucrose-induced obese rats". Experimental Biology and Medicine 229 (6): 486–93. June 2004. doi:10.1177/153537020422900606. PMID 15169967.
- ↑ 104.0 104.1 "Erythrocyte membrane fatty acids and subsequent breast cancer: a prospective Italian study". Journal of the National Cancer Institute 93 (14): 1088–95. July 2001. doi:10.1093/jnci/93.14.1088. PMID 11459870.
- ↑ 105.0 105.1 "Omega-3 Fatty Acids and Health: Fact Sheet for Health Professionals". US National Institutes of Health, Office of Dietary Supplements. 2 November 2016. http://ods.od.nih.gov/factsheets/Omega3FattyAcids-HealthProfessional/.
- ↑ "Marine fatty acid intake is associated with breast cancer prognosis". The Journal of Nutrition 141 (2): 201–6. February 2011. doi:10.3945/jn.110.128777. PMID 21178081.
- ↑ "Trans fatty acid-forming processes in foods: a review". Anais da Academia Brasileira de Ciências 79 (2): 343–50. June 2007. doi:10.1590/S0001-37652007000200015. PMID 17625687.
- ↑ "Trans fatty acid isomers and the trans-9/trans-11 index in fat containing foods". European Journal of Lipid Science and Technology 113 (10): 1281–1292. October 2011. doi:10.1002/ejlt.201100037. PMID 22164125.
- ↑ Kummerow, Fred August; Kummerow, Jean M. (2008). Cholesterol Won't Kill You, But Trans Fat Could. Trafford. ISBN 978-1-4251-3808-0.
- ↑ 110.0 110.1 110.2 110.3 110.4 Trans Fat Task Force (June 2006). TRANSforming the Food Supply. Trans Fat Task Force. ISBN 0-662-43689-X. http://www.hc-sc.gc.ca/fn-an/nutrition/gras-trans-fats/tf-ge/tf-gt_rep-rap_e.html. Retrieved 7 January 2007.
- ↑ "DIETA DETOX ✅ QUÉ ES Y SUS 13 PODEROSOS BENEFICIOS". October 24, 2019. https://mejorandomishabitos.es/dieta-detox/.
- ↑ 112.0 112.1 "New and existing oils and fats used in products with reduced trans-fatty acid content". Journal of the American Dietetic Association 106 (6): 867–80. June 2006. doi:10.1016/j.jada.2006.03.010. PMID 16720128.
- ↑ "Trans-fatty acids, dangerous bonds for health? A background review paper of their use, consumption, health implications and regulation in France". European Journal of Nutrition 52 (4): 1289–302. June 2013. doi:10.1007/s00394-012-0484-4. PMID 23269652.
- ↑ "Wilhelm Normann und die Geschichte der Fetthärtung von Martin Fiedler, 2001". 20 December 2011. http://www.dgfett.de/history/normann/nr_fiedler.htm.
- ↑ Gormley, James J.; Juturu, Vijaya (2010) (in en). Modern Dietary Fat Intakes in Disease Promotion. Nutrition and Health. Totowa, NJ: Humana Press. pp. 85–94. doi:10.1007/978-1-60327-571-2_5. ISBN 978-1-60327-571-2.
- ↑ 116.0 116.1 "Tentative Determination Regarding Partially Hydrogenated Oils". Federal Register. 8 November 2013. https://www.federalregister.gov/articles/2013/11/08/2013-26854/tentative-determination-regarding-partially-hydrogenated-oils-request-for-comments-and-for.
- ↑ Hill, John W.; Kolb, Doris K (2007). Chemistry for changing times. Pearson / Prentice Hall. ISBN 978-0-13-605449-8.
- ↑ Ashok, Chauhan; Ajit, Varma (2009). "Chapter 4: Fatty acids". A Textbook of Molecular Biotechnology. I. K. International Pvt. p. 181. ISBN 978-93-80026-37-4.
- ↑ 119.0 119.1 "Trans fatty acid isomers in human health and in the food industry". Biological Research 32 (4): 273–87. 1999. doi:10.4067/s0716-97601999000400007. PMID 10983247.
- ↑ "Heart Foundation: Butter has 20 times the trans fats of marg | Australian Food News". www.ausfoodnews.com.au. http://www.ausfoodnews.com.au/2010/09/28/heart-foundation-butter-has-20-times-the-trans-fats-of-marg.html.
- ↑ "Dietary levels of trans fatty acids" basis for health concerns and industry efforts to limit use". Nutrition Research 25 (5): 499–513. 2005. doi:10.1016/j.nutres.2005.04.002.
- ↑ "What's in that french fry? Fat varies by city". NBC News. 12 April 2006. https://www.nbcnews.com/id/12287818. AP story concerning Stender, S; Dyerberg, J; Astrup, A (April 2006). "High levels of industrially produced trans fat in popular fast foods". N. Engl. J. Med. 354 (15): 1650–2. doi:10.1056/NEJMc052959. PMID 16611965.
- ↑ "Fats and Cholesterol" , Harvard School of Public Health. Retrieved 02-11-16.
- ↑ 124.0 124.1 Food and nutrition board, institute of medicine of the national academies (2005). Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids (macronutrients). National Academies Press. pp. 423. doi:10.17226/10490. ISBN 978-0-309-08525-0. https://archive.org/details/isbn_9780309085250/page/423.
- ↑ 125.0 125.1 125.2 Food and nutrition board, institute of medicine of the national academies (2005). Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids (macronutrients). National Academies Press. p. 504. http://darwin.nap.edu/books/0309085373/html/504.html.[yes|permanent dead link|dead link}}]
- ↑ 126.0 126.1 126.2 126.3 126.4 Trans Fat Task Force (June 2006). TRANSforming the Food Supply. (Consultation on the health implications of alternatives to trans fatty acids: Summary of Responses from Experts)
- ↑ "Trans fatty acids: are the effects only marginal?". American Journal of Public Health 84 (5): 722–4. May 1994. doi:10.2105/AJPH.84.5.722. PMID 8179036.
- ↑ "Trans fatty acids and coronary heart disease". Nutrition in Clinical Practice 21 (5): 505–12. October 2006. doi:10.1177/0115426506021005505. PMID 16998148.
- ↑ 129.0 129.1 129.2 129.3 "Trans fatty acids and cardiovascular disease". The New England Journal of Medicine 354 (15): 1601–13. April 2006. doi:10.1056/NEJMra054035. PMID 16611951.
- ↑ 130.0 130.1 "Dietary fat intake and the risk of coronary heart disease in women". The New England Journal of Medicine 337 (21): 1491–9. November 1997. doi:10.1056/NEJM199711203372102. PMID 9366580.
- ↑ "Dietary fat intake and risk of coronary heart disease in women: 20 years of follow-up of the nurses' health study". American Journal of Epidemiology 161 (7): 672–9. April 2005. doi:10.1093/aje/kwi085. PMID 15781956.
- ↑ "Trans fatty acids and coronary heart disease". The New England Journal of Medicine 340 (25): 1994–8. June 1999. doi:10.1056/NEJM199906243402511. PMID 10379026.
- ↑ "Effect of dietary trans fatty acids on high-density and low-density lipoprotein cholesterol levels in healthy subjects". The New England Journal of Medicine 323 (7): 439–45. August 1990. doi:10.1056/NEJM199008163230703. PMID 2374566. http://library.wur.nl/WebQuery/wurpubs/13110.
- ↑ "Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials". The American Journal of Clinical Nutrition 77 (5): 1146–55. May 2003. doi:10.1093/ajcn/77.5.1146. PMID 12716665.
- ↑ "Postprandial effects of dietary trans fatty acids on apolipoprotein(a) and cholesteryl ester transfer". The American Journal of Clinical Nutrition 77 (5): 1119–24. May 2003. doi:10.1093/ajcn/77.5.1119. PMID 12716661.
- ↑ "Consumption of trans fatty acids is related to plasma biomarkers of inflammation and endothelial dysfunction". The Journal of Nutrition 135 (3): 562–6. March 2005. doi:10.1093/jn/135.3.562. PMID 15735094.
- ↑ "trans Fatty acids in human milk are inversely associated with concentrations of essential all-cis n-6 and n-3 fatty acids and determine trans, but not n-6 and n-3, fatty acids in plasma lipids of breast-fed infants". The American Journal of Clinical Nutrition 70 (3): 383–90. September 1999. doi:10.1093/ajcn/70.3.383. PMID 10479201.
- ↑ "Dietary fats and the risk of incident Alzheimer disease". Archives of Neurology 60 (2): 194–200. February 2003. doi:10.1001/archneur.60.2.194. PMID 12580703.
- ↑ 139.0 139.1 "High dietary consumption of trans fatty acids decreases brain docosahexaenoic acid but does not alter amyloid-beta and tau pathologies in the 3xTg-AD model of Alzheimer's disease". Neuroscience 159 (1): 296–307. March 2009. doi:10.1016/j.neuroscience.2008.12.006. PMID 19135506.
- ↑ "Effects of a saturated fat and high cholesterol diet on memory and hippocampal morphology in the middle-aged rat". Journal of Alzheimer's Disease 14 (2): 133–45. June 2008. doi:10.3233/JAD-2008-14202. PMID 18560126.
- ↑ American Cancer Society. "Common questions about diet and cancer". http://www.cancer.org/docroot/ped/content/ped_3_2x_common_questions_about_diet_and_cancer.asp.
- ↑ "A prospective study of blood trans fatty acid levels and risk of prostate cancer". Proc. Amer. Assoc. Cancer Res. 47 (1): 943. 1 April 2006. http://www.aacrmeetingabstracts.org/cgi/content/abstract/2006/1/943. Retrieved 9 January 2007.
- ↑ "Serum phospholipid fatty acids and prostate cancer risk: results from the prostate cancer prevention trial". American Journal of Epidemiology 173 (12): 1429–39. June 2011. doi:10.1093/aje/kwr027. PMID 21518693.
- ↑ "Breast cancer: a role for trans fatty acids?". World Health Organization (Press release). 11 April 2008. Archived from the original on 13 April 2008.
- ↑ "Association between serum trans-monounsaturated fatty acids and breast cancer risk in the E3N-EPIC Study". American Journal of Epidemiology 167 (11): 1312–20. June 2008. doi:10.1093/aje/kwn069. PMID 18390841.
- ↑ Riserus, Ulf (2006). "Trans fatty acids, insulin sensitivity and type 2 diabetes". Scandinavian Journal of Food and Nutrition 50 (4): 161–165. doi:10.1080/17482970601133114.
- ↑ "Diet and risk of Type II diabetes: the role of types of fat and carbohydrate". Diabetologia 44 (7): 805–17. July 2001. doi:10.1007/s001250100547. PMID 11508264.
- ↑ "Dietary fat and meat intake in relation to risk of type 2 diabetes in men". Diabetes Care 25 (3): 417–24. March 2002. doi:10.2337/diacare.25.3.417. PMID 11874924.
- ↑ Gosline, Anna (12 June 2006). "Why fast foods are bad, even in moderation". New Scientist. https://www.newscientist.com/article.ns?id=dn9318.
- ↑ "Six years of fast-food fats supersizes monkeys". New Scientist (2556): 21. 17 June 2006. https://www.newscientist.com/channel/health/mg19025565.000-six-years-of-fastfood-fats-supersizes-monkeys.html.
- ↑ 151.0 151.1 "Trans fat diet induces abdominal obesity and changes in insulin sensitivity in monkeys". Obesity 15 (7): 1675–84. July 2007. doi:10.1038/oby.2007.200. PMID 17636085.
- ↑ Thompson, Tommy G. "Trans Fat Press Conference". https://www.hhs.gov/news/speech/2003/030709.html., US Secretary of health and human services
- ↑ "Dietary fatty acid intakes and the risk of ovulatory infertility". The American Journal of Clinical Nutrition 85 (1): 231–7. January 2007. doi:10.1093/ajcn/85.1.231. PMID 17209201.
- ↑ Roan, Shari (28 January 2011). "Trans fats and saturated fats could contribute to depression". The Sydney Morning Herald. https://www.smh.com.au/lifestyle/wellbeing/food-with-bad-fats-linked-to-depression-study-finds-20110127-1a6vy.html.
- ↑ "Selective deficits in the omega-3 fatty acid docosahexaenoic acid in the postmortem orbitofrontal cortex of patients with major depressive disorder". Biological Psychiatry 62 (1): 17–24. July 2007. doi:10.1016/j.biopsych.2006.08.026. PMID 17188654. http://www.biologicalpsychiatryjournal.com/article/S0006-3223(06)01065-1/abstract.
- ↑ "Trans fat consumption and aggression". PLOS ONE 7 (3): e32175. 2012. doi:10.1371/journal.pone.0032175. PMID 22403632. Bibcode: 2012PLoSO...732175G.
- ↑ "A Fat to Forget: Trans Fat Consumption and Memory". PLOS ONE 10 (6): e0128129. 2015. doi:10.1371/journal.pone.0128129. PMID 26083739. Bibcode: 2015PLoSO..1028129G.
- ↑ Weinberg, Jeffrey, ed (15 July 2015). "Linking diet to acne metabolomics, inflammation, and comedogenesis: an update". Clinical, Cosmetic and Investigational Dermatology 8: 371–88. doi:10.2147/CCID.S69135. PMID 26203267.
- ↑ "Trans fatty acids in hydrogenated fat inhibited the synthesis of the polyunsaturated fatty acids in the phospholipid of arterial cells". Life Sciences 74 (22): 2707–23. April 2004. doi:10.1016/j.lfs.2003.10.013. PMID 15043986.
- ↑ Landis CR, Weinhold F. Origin of trans-bent geometries in maximally bonded transition metal and main group molecules. Journal of the American Chemical Society. 2006 Jun 7;128(22):7335-45.
- ↑ "Influence of trans fatty acids on infant and fetus development". Acta Microbiologica Polonica 52 Suppl: 67–74. 2003. PMID 15058815.
- ↑ "Metabolic aspects of trans fatty acids". Clinical Nutrition 16 (5): 229–37. October 1997. doi:10.1016/s0261-5614(97)80034-9. PMID 16844601.
- ↑ "Effect of dietary trans fatty acids on the delta 5, delta 6 and delta 9 desaturases of rat liver microsomes in vivo". Acta Biologica et Medica Germanica 40 (12): 1699–1705. 1981. PMID 7345825.
- ↑ "National Nutrient Database for Standard Reference Release 28". United States Department of Agriculture. https://ndb.nal.usda.gov/ndb/foods/show/1?fgcd=&manu=&lfacet=&format=&count=&max=50&offset=50&sort=default&order=asc&qlookup=butter&ds=&qt=&qp=&qa=&qn=&q=&ing=.[|permanent dead link|dead link}}]
- ↑ National Dairy Council (18 June 2004). "comments on 'Docket No. 2003N-0076 Food Labeling: Trans Fatty Acids in Nutrition Labeling'". https://www.fda.gov/ohrms/dockets/dailys/04/June04/062304/03N-0076-emc00228-01.pdf.
- ↑ Reitsma, Pieter H, ed (March 2010). "Effect of animal and industrial trans fatty acids on HDL and LDL cholesterol levels in humans--a quantitative review". PLOS ONE 5 (3): e9434. doi:10.1371/journal.pone.0009434. PMID 20209147. Bibcode: 2010PLoSO...5.9434B.
- ↑ "Opposing effects of cis-9,trans-11 and trans-10,cis-12 conjugated linoleic acid on blood lipids in healthy humans". The American Journal of Clinical Nutrition 80 (3): 614–20. September 2004. doi:10.1093/ajcn/80.3.614. PMID 15321800.
- ↑ "Inflammation and conjugated linoleic acid: mechanisms of action and implications for human health". Journal of Physiology and Biochemistry 61 (3): 483–94. September 2005. doi:10.1007/BF03168454. PMID 16440602.
- ↑ Trans Fats From Ruminant Animals May Be Beneficial – Health News . redOrbit (8 September 2011). Retrieved 22 January 2013.
- ↑ "Dietary vaccenic acid has antiatherogenic effects in LDLr-/- mice". The Journal of Nutrition 140 (1): 18–24. January 2010. doi:10.3945/jn.109.105163. PMID 19923390.
- ↑ "Beneficial effects of vaccenic acid on postprandial lipid metabolism and dyslipidemia: Impact of natural trans-fats to improve CVD risk". Lipid Technology 22 (5): 103–106. 20 May 2010. doi:10.1002/lite.201000016.
- ↑ David J. Baer, PhD. US Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Laboratory. New Findings on Dairy Trans Fat and Heart Disease Risk, IDF World Dairy Summit 2010, 8–11 November 2010. Auckland, New Zealand
- ↑ ((EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA))) (2010). "Scientific opinion on dietary reference values for fats". EFSA Journal 8 (3): 1461. doi:10.2903/j.efsa.2010.1461.
- ↑ UK Scientific Advisory Committee on Nutrition (2007). "Update on trans fatty acids and health, Position Statement". http://www.food.gov.uk/multimedia/pdfs/board/fsa071207.pdf.
- ↑ "Effect of animal and industrial trans fatty acids on HDL and LDL cholesterol levels in humans--a quantitative review". PLOS ONE 5 (3): e9434. March 2010. doi:10.1371/journal.pone.0009434. PMID 20209147. Bibcode: 2010PLoSO...5.9434B.
- ↑ "Trans fat". Health Canada. Dec 2007. http://www.hc-sc.gc.ca/hl-vs/iyh-vsv/food-aliment/trans-eng.php.
- ↑ "EFSA sets European dietary reference values for nutrient intakes" (Press release). European Food Safety Authority. 26 March 2010.
- ↑ "WHO plan to eliminate industrially-produced trans-fatty acids from global food supply" (Press release). World Health Organization. 14 May 2018.
- ↑ Food and nutrition board, institute of medicine of the national academies (2005). Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academies Press. p. i. http://darwin.nap.edu/books/0309085373/html/R1.html.
- ↑ Summary .
- ↑ Food and nutrition board, institute of medicine of the national academies (2005). Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academies Press. p. 447. http://darwin.nap.edu/books/0309085373/html/447.html.[yes|permanent dead link|dead link}}]
- ↑ Food and nutrition board, institute of medicine of the national academies (2005). Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). National Academies Press. p. 424. http://darwin.nap.edu/books/0309085373/html/424.html.[yes|permanent dead link|dead link}}]
- ↑ "Preparation of spread oils meeting U.S. Food and Drug Administration Labeling requirements for trans fatty acids via pressure-controlled hydrogenation". Journal of Agricultural and Food Chemistry 53 (15): 5982–4. July 2005. doi:10.1021/jf047849+. PMID 16028984.
- ↑ Hadzipetros, Peter (25 January 2007). "Trans Fats Headed for the Exit". CBC News. http://www.cbc.ca/health/fitness-blog/2007/01/trans_fats_headed_for_the_exit.html.
- ↑ Spencelayh, Michael (9 January 2007). "Trans fat free future". http://www.rsc.org/Publishing/ChemScience/Volume/2007/02/trans_fat_free_future.asp.
- ↑ "Effect of fish oil on cognitive performance in older subjects: a randomized, controlled trial". Neurology 71 (6): 430–8. August 2008. doi:10.1212/01.wnl.0000324268.45138.86. PMID 18678826.
- ↑ Mensink, Ronald P.; Sanders, Thomas A.; Baer, David J.; Hayes, K. C.; Howles, Philip N.; Marangoni, Alejandro (2016-07-01). "The Increasing Use of Interesterified Lipids in the Food Supply and Their Effects on Health Parameters" (in en). Advances in Nutrition 7 (4): 719–729. doi:10.3945/an.115.009662. ISSN 2161-8313. PMID 27422506.
- ↑ "Positional distribution of fatty acids in dietary triglycerides: effects on fasting blood lipoprotein concentrations in humans.", Am J Clin Nutr 61 (1): pp. 48–551, 1995, doi:10.1093/ajcn/61.1.48, PMID 7825538, http://www.ajcn.org/cgi/reprint/61/1/48.pdf
- ↑ "Effect on plasma lipids of interesterifying a mix of edible oils.", Am J Clin Nutr 62 (5): pp. 950–55, 1995, doi:10.1093/ajcn/62.5.950, PMID 7572740, http://www.ajcn.org/cgi/reprint/62/5/950.pdf
- ↑ "Interesterification of fats in margarine: effect on blood lipids, blood enzymes and hemostasis parameters.", Eur J Clin Nutr 51 (8): pp. 527–34, 1997, doi:10.1038/sj.ejcn.1600437, PMID 11248878
- ↑ "Comparison of effects of palmitic and stearic acids in the diet on serum cholesterol in man.", Am J Clin Nutr 23 (9): pp. 1184–93, 1970, doi:10.1093/ajcn/23.9.1184, PMID 5450836, http://www.ajcn.org/cgi/reprint/23/9/1184.pdf
- ↑ "The solid fat content of stearic acid-rich fats determines their postprandial effects.", Am J Clin Nutr 85 (6): pp. 1486–94, 2007, doi:10.1093/ajcn/85.6.1486, PMID 17556683, http://www.ajcn.org/cgi/reprint/85/6/1486.pdf
- ↑ "The effect of triacylglycerol fatty acids positional distribution on postprandial plasma metabolite and hormone responses in normal adult men.", Br J Nutr 71 (3): pp. 401–10, 1994, doi:10.1079/bjn19940147, PMID 8172869
- ↑ "Effects of palm oil and transesterified palm oil on chylomicron and VLDL triacylglycerol structures and postprandial lipid response.", J Lipid Res 42 (10): pp. 1618–25, 2001, PMID 11590218, http://www.jlr.org/cgi/reprint/42/10/1618.pdf
- ↑ "Effect of interesterification of palmitic-acid rich tryacylglycerol on postprandial lipid and factor VII response", Lipids 42 (4): 315–323, 2007, doi:10.1007/s11745-007-3024-x, PMID 17406926
- ↑ "Use of structured triacylglycerols containing predominantly stearic and oleic acids to probe early events in metabolic processing of dietary fat", J Lipid Res 40 (10): pp. 1890–98, 1999, PMID 10508209, http://www.jlr.org/cgi/reprint/40/10/1890.pdf
- ↑ "Substituting enzymically interesterified butter for native butter has no effect on lipemia or lipoproteinemia in man", Annals of Nutrition and Metabolism 44 (2): 61–67, 2000, doi:10.1159/000012822, PMID 10970994
- ↑ "Stearic acid-rich interesterified fat and trans-rich fat raise the LDL/HDL ratio and plasma glucose relative to palm olein in humans". Nutr Metab 4: 3. 2007. doi:10.1186/1743-7075-4-3. PMID 17224066. PMC 1783656. http://www.nutritionandmetabolism.com/content/pdf/1743-7075-4-3.pdf. Retrieved 2007-01-19.
- ↑ "Letter to the editor: healthy alternatives to trans fats", Nutr Metab 4: p. 10, 2007, doi:10.1186/1743-7075-4-10, PMID 17462099
- ↑ "Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials.", Am J Clin Nutr 77 (5): pp. 1146–1155, 2003, doi:10.1093/ajcn/77.5.1146, PMID 12716665, http://www.ajcn.org/cgi/reprint/77/5/1146.pdf
- ↑ "Boston scientists say triglycerides play key role in heart health". The Boston Globe. https://www.bostonglobe.com/news/science/2014/06/18/boston-researchers-find-that-triglycerides-play-pivotal-role-heart-health/ynrM4QQwIq1fCCoRwMfOAN/story.html.
- ↑ "Small Dense Low-Density Lipoprotein as Biomarker for Atherosclerotic Diseases". Oxidative Medicine and Cellular Longevity 2017: 1273042. 2017. doi:10.1155/2017/1273042. PMID 28572872.
- ↑ "Triglycerides". https://www.nlm.nih.gov/medlineplus/ency/article/003493.htm.
- ↑ Crawford, H., Micheal. Current Diagnosis & Treatment Cardiology. 3rd ed. McGraw-Hill Medical, 2009. p19
- ↑ "What's considered normal?". Mayo Clinic. 28 September 2012. http://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/in-depth/triglycerides/art-20048186.
- ↑ 206.0 206.1 Nordestgaard, BG; Varbo, A (August 2014). "Triglycerides and cardiovascular disease". The Lancet 384 (9943): 626–35. doi:10.1016/S0140-6736(14)61177-6. PMID 25131982.
- ↑ GILL, Jason; Sara HERD; Natassa TSETSONIS; Adrianne HARDMAN (Feb 2002). "Are the reductions in triacylglycerol and insulin levels after exercise related?". Clinical Science 102 (2): 223–231. doi:10.1042/cs20010204. PMID 11834142. http://www.clinsci.org/cs/102/0223/cs1020223.htm. Retrieved 2 March 2013.
- ↑ 208.0 208.1 Crawford, H., Micheal. Current Diagnosis & Treatment Cardiology. 3rd ed. McGraw-Hill Medical, 2009. p21
- ↑ 209.0 209.1 209.2 "Evaluation and treatment of hypertriglyceridemia: an endocrine society clinical practice guideline". J. Clin. Endocrinol. Metab. 97 (9): 2969–89. September 2012. doi:10.1210/jc.2011-3213. PMID 22962670.
- ↑ Davidson, Michael H. (28 January 2008). "Pharmacological Therapy for Cardiovascular Disease". in Davidson, Michael H.; Toth, Peter P.; Maki, Kevin C.. Therapeutic Lipidology. Contemporary Cardiology. Cannon, Christopher P.; Armani, Annemarie M.. Totowa, New Jersey: Humana Press, Inc.. pp. 141–142. ISBN 978-1-58829-551-4.
- ↑ "Effect of fibrates on lipid profiles and cardiovascular outcomes: a systematic review". Am J Med 122 (10): 962.e1–962.e8. 2009. doi:10.1016/j.amjmed.2009.03.030. PMID 19698935.
- ↑ "Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis". Lancet 375 (9729): 1875–1884. 2010. doi:10.1016/S0140-6736(10)60656-3. PMID 20462635.
- ↑ Blair, HA; Dhillon, S (Oct 2014). "Omega-3 carboxylic acids: a review of its use in patients with severe hypertriglyceridemia". Am J Cardiovasc Drugs 14 (5): 393–400. doi:10.1007/s40256-014-0090-3. PMID 25234378.
- ↑ Panov, Alexander; Orynbayeva, Zulfiya; Vavilin, Valentin; Lyakhovich, Vyacheslav (2014). Baranova, Ancha. ed. "Fatty Acids in Energy Metabolism of the Central Nervous System". BioMed Research International (Hindawa) 2014 (The Roads to Mitochondrial Dysfunction): 472459. doi:10.1155/2014/472459. PMID 24883315.
 |