Chemistry:Vitamin D
| Vitamin D | |
|---|---|
| Drug class | |
 Cholecalciferol (D3) | |
| Class identifiers | |
| Synonyms | Calciferols |
| Use | Rickets, osteoporosis, vitamin D deficiency |
| ATC code | A11CC |
| Biological target | vitamin D receptor |
| Clinical data | |
| Drugs.com | MedFacts Natural Products |
| External links | |
| MeSH | D014807 |
Vitamin D is a group of fat-soluble secosteroids responsible for increasing intestinal absorption of calcium, magnesium, and phosphate, and for many other biological effects.[1][2][3] In humans, the most important compounds in this group are vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol).[2][3][4]
The major natural source of vitamin D is synthesis of cholecalciferol in the lower layers of the epidermis of the skin, through a photochemical reaction with Ultraviolet B (UV-B) radiation from sun exposure or UV-B lamps.[1] Cholecalciferol and ergocalciferol can be ingested from the diet and supplements.[1][2] Only a few foods, such as the flesh of fatty fish, naturally contain significant amounts of vitamin D.[2][5] In the U.S. and other countries, cow's milk and plant-derived milk substitutes are fortified with vitamin D, as are many breakfast cereals.[1] Mushrooms exposed to ultraviolet light contribute useful amounts of vitamin D2.[2] [6]Dietary recommendations typically assume that all of a person's vitamin D is taken by mouth, because sun exposure in the population is variable and recommendations about the amount of sun exposure that is safe are uncertain in view of the skin cancer risk.[2]
Vitamin D from the diet, or from skin synthesis, is biologically inactive. It is activated by two protein enzyme hydroxylation steps, the first in the liver and the second in the kidneys.[1][4] Because vitamin D can be synthesized in adequate amounts by most mammals if they get enough sunlight, it is not essential and therefore is technically not a vitamin.[3] Instead it can be considered a hormone, with activation of the vitamin D pro-hormone resulting in the active form, calcitriol, which then produces effects via a nuclear receptor in multiple locations.[3]
Cholecalciferol is converted in the liver to calcifediol (25-hydroxycholecalciferol); ergocalciferol is converted to 25-hydroxyergocalciferol.[1] These two vitamin D metabolites (called 25-hydroxyvitamin D or 25(OH)D) are measured in serum to determine a person's vitamin D status.[7][8] Calcifediol is further hydroxylated by the kidneys and some of the immune system cells to form calcitriol (1,25-dihydroxycholecalciferol), the biologically active form of vitamin D.[9][10] Calcitriol circulates as a hormone in the blood, having a major role regulating the concentration of calcium and phosphate, and promoting the healthy growth and remodeling of bone.[1] Calcitriol also has other effects, including some on cell growth, neuromuscular and immune functions, and reduction of inflammation.[2]
Vitamin D has a significant role in calcium homeostasis and metabolism.[1] Its discovery was due to effort to find the dietary substance lacking in children with rickets (the childhood form of osteomalacia).[11] Vitamin D supplements are given to treat or to prevent osteomalacia and rickets.[1] The evidence for other health effects of vitamin D supplementation in vitamin D–replete individuals is inconsistent.[2] The effect of vitamin D supplementation on mortality is not clear, with one meta-analysis finding a small decrease in mortality in elderly people.[12] Except for the prevention of rickets and osteomalacia in high-risk groups, any benefit of vitamin D supplements to musculoskeletal or general health may be small.[13][14][15]
Types
| Name | Chemical composition | Structure |
|---|---|---|
| Vitamin D1 | Mixture of molecular compounds of ergocalciferol with lumisterol, 1:1 | |
| Vitamin D2 | ergocalciferol (made from ergosterol) | 
|
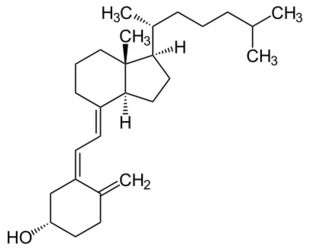
| Vitamin D3 | cholecalciferol
(made from 7-dehydrocholesterol in the skin). |

|
| Vitamin D4 | 22-dihydroergocalciferol | 
|
| Vitamin D5 | sitocalciferol
(made from 7-dehydrositosterol) |

|
Several forms (vitamers) of vitamin D exist.[1] The two major forms are vitamin D2 or ergocalciferol, and vitamin D3 or cholecalciferol.[1] Vitamin D without a subscript refers to either D2 or D3, or both, and is known collectively as calciferol.[citation needed]
Vitamin D2 was chemically characterized in 1931. In 1935, the chemical structure of vitamin D3 was defined and shown to result from the ultraviolet irradiation of 7-dehydrocholesterol. A chemical nomenclature for vitamin D forms was recommended in 1981,[16] but alternative names remain in common use.[4]
Chemically, the various forms of vitamin D are secosteroids, that is, steroids in which one of the bonds in the steroid rings is broken.[17] The structural difference between vitamin D2 and vitamin D3 is in the side chain, which contains a double bond, between carbons 22 and 23, and a methyl group on carbon 24 in vitamin D2.[4] Many vitamin D analogues have been synthesized.[4]
Biology

The active vitamin D metabolite calcitriol mediates its biological effects by binding to the vitamin D receptor (VDR), which is principally located in the nuclei of target cells.[1][17] The binding of calcitriol to the VDR allows the VDR to act as a transcription factor that modulates the gene expression of transport proteins (such as TRPV6 and calbindin), which are involved in calcium absorption in the intestine.[19] The vitamin D receptor belongs to the nuclear receptor superfamily of steroid/thyroid hormone receptors, and VDRs are expressed by cells in most organs, including the brain, heart, skin, gonads, prostate and breast.
VDR activation in the intestine, bone, kidney, and parathyroid gland cells leads to the maintenance of calcium and phosphorus levels in the blood (with the assistance of parathyroid hormone and calcitonin) and to the maintenance of bone content.[1][20]
One of the most important roles of vitamin D is to maintain skeletal calcium balance by promoting calcium absorption in the intestines, promoting bone resorption by increasing osteoclast number, maintaining calcium and phosphate levels for bone formation, and allowing proper functioning of parathyroid hormone to maintain serum calcium levels.[1] Vitamin D deficiency can result in lower bone mineral density and an increased risk of reduced bone density (osteoporosis) or bone fracture because a lack of vitamin D alters mineral metabolism in the body.[1][21] Thus, vitamin D is also critical for bone remodeling through its role as a potent stimulator of bone resorption.[21]
The VDR regulates cell proliferation and differentiation. Vitamin D also affects the immune system, and VDRs are expressed in several white blood cells, including monocytes and activated T and B cells.[22] In vitro, vitamin D increases expression of the tyrosine hydroxylase gene in adrenal medullary cells, and affects the synthesis of neurotrophic factors, nitric oxide synthase, and glutathione.[23]
Vitamin D receptor expression decreases with age.[1]
Deficiency
A diet with insufficient vitamin D in conjunction with inadequate sun exposure causes vitamin D deficiency, which is defined as a blood 25(OH)D level below 12 ng/mL (30 nmol/liter), whereas vitamin D insufficiency is a blood 25(OH)D level of 12–20 ng/mL (30–50 nmol/liter).[2][24] An estimated one billion adults worldwide are either vitamin D insufficient or deficient,[25] including in developed countries in Europe.[26] Severe vitamin D deficiency in children, a rare disease in the developed world, causes a softening and weakening of growing bones, and a condition called rickets.[27]
Vitamin D deficiency is found worldwide in the elderly and remains common in children and adults.[28][29][25] Deficiency results in impaired bone mineralization and bone damage which leads to bone-softening diseases,[30] including rickets in children and osteomalacia in adults. Low blood calcifediol (25-hydroxy-vitamin D) can result from avoiding the sun.[31] Being deficient in Vitamin D can cause the absorption of dietary calcium to fall from the normal fraction (between 60 and 80 percent) to as little as 15 percent.[20]
Dark-skinned people living in temperate climates have been shown to have low vitamin D levels.[32][33][34] Dark-skinned people are less efficient at making vitamin D because melanin in the skin hinders vitamin D synthesis.[35] Vitamin D deficiency is common in Hispanic and African-Americans in the United States, with levels dropping significantly in the winter.[24] This is due to the levels of melanin in the skin, as it acts as a natural protectant from sun exposure.[24]
Bone health
Rickets
Rickets, a childhood disease, is characterized by impeded growth and soft, weak, deformed long bones that bend and bow under their weight as children start to walk. Rickets typically appears between 3 and 18 months of age.[36] Cases continue to be reported in North American and other Western Countries and is primarily seen in breastfed infants and those with darker skin complexions.[36] This condition is characterized by bow legs,[30] which can be caused by calcium or phosphorus deficiency, as well as a lack of vitamin D; in the 21st century, it is largely found in low-income countries in Africa, Asia, or the Middle East[37] and in those with genetic disorders such as pseudo-vitamin-D-deficiency rickets.[38]
Maternal vitamin D deficiency may cause overt bone disease from before birth and impairment of bone quality after birth.[39][40] Nutritional rickets exists in countries with intense year-round sunlight such as Nigeria and can occur without vitamin D deficiency.[41][42]
Although rickets and osteomalacia are now rare in the United Kingdom, outbreaks have happened in some immigrant communities in which people with osteomalacia included women with seemingly adequate daylight outdoor exposure wearing Western clothing.[43] Having darker skin and reduced exposure to sunshine did not produce rickets unless the diet deviated from a Western omnivore pattern characterized by high intakes of meat, fish, and eggs.[44][45][46] The dietary risk factors for rickets include abstaining from animal foods.[43][47]
Vitamin D deficiency remains the main cause of rickets among young infants in most countries because breast milk is low in vitamin D and social customs and climatic conditions can prevent adequate sun exposure. In sunny countries such as Nigeria, South Africa, and Bangladesh, where rickets occurs among older toddlers and children, it has been attributed to low dietary calcium intakes, which are characteristic of cereal-based diets with limited access to dairy products.[46]
Rickets was formerly a major public health problem among the US population. In Denver, almost two-thirds of 500 children had mild rickets in the late 1920s.[48] An increase in the proportion of animal protein[47][49] in the 20th century American diet coupled with increased consumption of milk[50][51] fortified with relatively small quantities of vitamin D coincided with a dramatic decline in the number of rickets cases.[20] Also, in the United States and Canada, vitamin D-fortified milk, infant vitamin supplements, and vitamin supplements have helped to eradicate the majority of cases of rickets for children with fat malabsorption conditions.[30]
Osteomalacia and osteoporosis
Osteomalacia is a disease in adults that results from vitamin D deficiency.[1] Characteristics of this disease are softening of the bones, leading to bending of the spine, proximal muscle weakness, bone fragility, and increased risk for fractures.[1] Osteomalacia reduces calcium absorption and increases calcium loss from bone, which increases the risk for bone fractures. Osteomalacia is usually present when 25-hydroxyvitamin D levels are less than about 10 ng/mL.[52] Although the effects of osteomalacia are thought to contribute to chronic musculoskeletal pain, there is no persuasive evidence of lower vitamin D levels in people with chronic pain[53] or that supplementation alleviates chronic nonspecific musculoskeletal pain.[54] Osteomalacia progress to osteoporosis, a condition of reduced bone mineral density with increased bone fragility and risk of bone fractures. Osteoporosis can be a long-term effect of calcium and/or vitamin D insufficiency, the latter contributing by reducing calcium absorption.[2]
Use of supplements
Supplementation with vitamin D is a reliable method for preventing or treating rickets.[1] On the other hand, the effects of vitamin D supplementation on non-skeletal health are uncertain.[55][56] A review did not find any effect from supplementation on the rates of non-skeletal disease, other than a tentative decrease in mortality in the elderly.[57] Vitamin D supplements do not alter the outcomes for myocardial infarction, stroke or cerebrovascular disease, cancer, bone fractures or knee osteoarthritis.[14][58]
A US Institute of Medicine (IOM) report states: "Outcomes related to cancer, cardiovascular disease and hypertension, and diabetes and metabolic syndrome, falls and physical performance, immune functioning and autoimmune disorders, infections, neuropsychological functioning, and preeclampsia could not be linked reliably with intake of either calcium or vitamin D, and were often conflicting."[59]:5 Some researchers claim the IOM was too definitive in its recommendations and made a mathematical mistake when calculating the blood level of vitamin D associated with bone health.[60] Members of the IOM panel maintain that they used a "standard procedure for dietary recommendations" and that the report is solidly based on the data.[60]
Mortality, all-causes
Vitamin D3 supplementation has been tentatively found to lead to a reduced risk of death in the elderly,[12][57] but the effect has not been deemed pronounced, or certain enough, to make taking supplements recommendable.[14] Other forms (vitamin D2, alfacalcidol, and calcitriol) do not appear to have any beneficial effects with regard to the risk of death.[12] High blood levels appear to be associated with a lower risk of death, but it is unclear if supplementation can result in this benefit.[61] Both an excess and a deficiency in vitamin D appear to cause abnormal functioning and premature aging.[62][63][64] The relationship between serum calcifediol concentrations and all-cause mortality is "U-shaped": mortality is elevated at high and low calcifediol levels, relative to moderate levels.[59] Harm from vitamin D appears to occur at a lower vitamin D level in the black population than in the white population.[59]:435
Bone health
In general, no good evidence supports the commonly held belief that vitamin D supplements can help prevent osteoporosis.[14] Its general use for prevention of this disease in those without vitamin D deficiency is thus likely not needed.[13] For older people with osteoporosis, taking vitamin D with calcium may help prevent hip fractures, but it also slightly increases the risk of stomach and kidney problems.[65] A study found that supplementation with 800 IU or more daily, in those older than 65 years was "somewhat favorable in the prevention of hip fracture and non-vertebral fracture".[66] The effect is small or none for people living independently.[67][68] Low serum vitamin D levels have been associated with falls, and low bone mineral density.[69] Taking extra vitamin D, however, does not appear to change the risk.[70]
Athletes who are vitamin D deficient are at an increased risk of stress fractures and/or major breaks, particularly those engaging in contact sports. The greatest benefit with supplementation is seen in athletes who are deficient (25(OH)D serum levels <30 ng/mL), or severely deficient (25(OH)D serum levels <25 ng/mL). Incremental decreases in risks are observed with rising serum 25(OH)D concentrations plateauing at 50 ng/mL with no additional benefits seen in levels beyond this point.[71]
A 2020 Cochrane systematic review has found limited evidence that vitamin D plus calcium, but not independently can improve healing in children with nutritional rickets, but the evidence was not conclusive for reducing fractures.[72]
The US Food and Drug Administration (FDA) has required manufacturers to declare the amount of vitamin D on nutrition facts labels, as "nutrients of public health significance", since May 2016. By a proposed deadline extension, some manufacturers had until 1 July 2021, to comply.[73]
Cancer
Potential associations have been found between low vitamin D levels and the risk of developing several types of cancer.[74][75] Meta-analyses of observational studies have found reduced risk of cancer incidence related to vitamin D intake and 25(OH)D levels, particularly for colorectal cancer, although the strength of the associations was classified as weak.[75][76] While randomized controlled trials have not confirmed that vitamin D supplements reduce the risk of cancer incidence, the relative risk of cancer deaths was lower by up to 16% in several meta-analyses.[77][76]
Cardiovascular disease
Vitamin D supplementation is not associated with a reduced risk of stroke, cerebrovascular disease, myocardial infarction, or ischemic heart disease.[14][78][79] Supplementation does not lower blood pressure in the general population.[80][81][82]
Immune system
Infectious diseases
In general, vitamin D functions to activate the innate and dampen the adaptive immune systems with antibacterial, antiviral and anti-inflammatory effects.[83][84] Low levels of vitamin D appear to be a risk factor for tuberculosis,[85] and historically it was used as a treatment.[86]
Vitamin D supplementation in low doses (400 to 1000 IU/day) may slightly decrease the overall risk of acute respiratory tract infections.[87] The benefits were found in young children and adolescents (ages 1 up to 16 years) and were not confirmed with higher doses (>1000 IU per day or more).[87] Vitamin D supplementation substantially reduces the rate of moderate or severe exacerbations of COPD in people with baseline 25(OH)D levels under 25nmol/L, but not in those with less severe deficiency.[88]
Asthma
Vitamin D supplementation does not help prevent asthma attacks or alleviate their symptoms.[89]
Inflammatory bowel disease
Low levels of vitamin D are associated with two major forms of human inflammatory bowel disease: Crohn's disease and ulcerative colitis.[90] Deficiencies in vitamin D have been linked to the severity of the case of inflammatory bowl disease, however, whether vitamin D deficiency causes inflammatory bowl disease or is a symptom of the disease is not clear.[91]
There is some evidence that vitamin D supplementation therapy for people with inflammatory bowel disease may be associated with improvements in scores for clinical inflammatory bowel disease activity and biochemical markers.[92] [91] Vitamin D treatment may be associated with less frequent relapse of symptoms in IBD.[91] It is not clear if this treatment improves the person's quality of life or what the clinical response to vitamin D treatment.[91] The ideal treatment regime and dose of vitamin D therapy has not been well enough studied.[91]
Other conditions
Diabetes
A meta-analysis reported that vitamin D supplementation significantly reduced the risk of type 2 diabetes for non-obese people with prediabetes.[93] Another meta-analysis reported that vitamin D supplementation significantly improved glycemic control [homeostatic model assessment-insulin resistance (HOMA-IR)], hemoglobin A1C (HbA1C), and fasting blood glucose (FBG) in individuals with type 2 diabetes.[94] In prospective studies, high versus low level of vitamin D was respectively associated with significant decrease in risk of type 2 diabetes, combined type 2 diabetes and prediabetes, and prediabetes.[95] A 2011 Cochrane systematic review examined one study that showed vitamin D together with insulin maintained levels of fasting C-peptide after 12 months better than insulin alone. However, it is important to highlight that the studies available to be included in this review presented considerable flaws in quality and design.[96]
Attention deficit hyperactivity disorder (ADHD)
A meta-analysis of observational studies showed that children with ADHD have lower vitamin D levels, and that there was a small association between low vitamin D levels at the time of birth and later development of ADHD.[97] Several small, randomized controlled trials of vitamin D supplementation indicated improved ADHD symptoms such as impulsivity and hyperactivity.[98]
Depression
Clinical trials of vitamin D supplementation for depressive symptoms have generally been of low quality and show no overall effect, although subgroup analysis showed supplementation for participants with clinically significant depressive symptoms or depressive disorder had a moderate effect.[99]
Cognition and dementia
A systematic review of clinical studies found an association between low vitamin D levels with cognitive impairment and a higher risk of developing Alzheimer's disease. However, lower vitamin D concentrations are also associated with poor nutrition and spending less time outdoors. Therefore, alternative explanations for the increase in cognitive impairment exist and hence a direct causal relationship between vitamin D levels and cognition could not be established.[100]
Schizophrenia
Trials have demonstrated lower vitamin D levels are highly prevalent in people with schizophrenia, particularly those with acute episodes.[101]
Pregnancy
Low levels of vitamin D in pregnancy are associated with gestational diabetes, pre-eclampsia, and small (for gestational age) infants.[102] Although taking vitamin D supplements during pregnancy raises blood levels of vitamin D in the mother at term,[103] the full extent of benefits for the mother or baby is unclear.[102][103][104] Pregnant women who take an adequate amount of vitamin D during gestation may experience a lower risk of pre-eclampsia[105] and positive immune effects.[106] Vitamin D supplementation is also likely to reduce the risk of gestational diabetes, undersized babies[105] and of their poor rate of growth.[107] Pregnant women often do not take the recommended amount of vitamin D.[106]
Weight loss
Though hypothesized that vitamin D supplementation may be an effective treatment for obesity apart from calorie restriction, one systematic review found no association of supplementation with body weight or fat mass.[108] A 2016 meta-analysis found that circulating vitamin D status was improved by weight loss, indicating that fat mass may be inversely associated with blood levels of vitamin D.[109]
Allowable health claims
Governmental regulatory agencies stipulate for the food and dietary supplement industries certain health claims as allowable as statements on packaging.
European Food Safety Authority
- normal function of the immune system[110]
- normal inflammatory response[110]
- normal muscle function[110]
- reduced risk of falling in people over age 60[111]
US Food and Drug Administration (FDA)
- "Adequate calcium and vitamin D, as part of a well balanced diet, along with physical activity, may reduce the risk of osteoporosis."[112]
- "Adequate calcium and regular exercise may help to achieve strong bones in children and adolescents and may reduce the risk of osteoporosis in older adults. An adequate intake of vitamin D is also necessary."[113]
Other possible agencies with claim guidance: Japan FOSHU[114] and Australia-New Zealand.[115]
Dietary intake
| United Kingdom | ||
| Age group | Intake (μg/day) | Maximum intake (μg/day)[116] |
|---|---|---|
| Breast-fed infants 0–12 months | 8.5 – 10 | 25 |
| Formula-fed infants (<500 mL/d) | 10 | 25 |
| Children 1 – 10 years | 10 | 50 |
| Children >10 and adults | 10 | 100 |
| United States | ||
| Age group | RDA (IU/day) | (μg/day)[59] |
| Infants 0–6 months | 400* | 10 |
| Infants 6–12 months | 400* | 10 |
| 1–70 years | 600 | 15 |
| Adults > 70 years | 800 | 20 |
| Pregnant/Lactating | 600 | 15 |
| Age group | Tolerable upper intake level (IU/day) | (μg/day) |
| Infants 0–6 months | 1,000 | 25 |
| Infants 6–12 months | 1,500 | 37.5 |
| 1–3 years | 2,500 | 62.5 |
| 4–8 years | 3,000 | 75 |
| 9+ years | 4,000 | 100 |
| Pregnant/lactating | 4,000 | 100[59] |
| Canada | ||
| Age group | RDA (IU)[117] | Tolerable upper intake (IU)[117] |
| Infants 0–6 months | 400* | 1,000 |
| Infants 7–12 months | 400* | 1,500 |
| Children 1–3 years | 600 | 2,500 |
| Children 4–8 years | 600 | 3,000 |
| Children and adults 9–70 years | 600 | 4,000 |
| Adults > 70 years | 800 | 4,000 |
| Pregnancy & lactation | 600 | 4,000 |
| Australia and New Zealand | ||
| Age group | Adequate Intake (μg)[115] | Upper Level of Intake (μg)[115] |
| Infants 0–12 months | 5* | 25 |
| Children 1–18 years | 5* | 80 |
| Adults 19–50 years | 5* | 80 |
| Adults 51–70 years | 10* | 80 |
| Adults > 70 years | 15* | 80 |
| European Food Safety Authority | ||
| Age group | Adequate Intake (μg)[118] | Tolerable upper limit (μg)[119] |
| Infants 0–12 months | 10 | 25 |
| Children 1–10 years | 15 | 50 |
| Children 11–17 years | 15 | 100 |
| Adults | 15 | 100 |
| Pregnancy & Lactation | 15 | 100 |
| * Adequate intake, no RDA/RDI yet established | ||
Recommended levels
Various institutions have proposed different recommendations for the amount of daily intake[120] of vitamin D. These vary according to precise definition, age, pregnancy or lactation, and the extent assumptions are made regarding skin synthesis of vitamin D.[116][59][117][115][118] Conversion: 1 μg (microgram) = 40 IU (international unit).[116]
United Kingdom
The UK National Health Service (NHS) recommends that people at risk of vitamin D deficiency, breast-fed babies, formula-fed babies taking less than 500 ml/day, and children aged 6 months to 4 years, should take daily vitamin D supplements throughout the year to ensure sufficient intake.[116] This includes people with limited skin synthesis of vitamin D, who are not often outdoors, are frail, housebound, living in a care home, or usually wearing clothes that cover up most of the skin, or with dark skin, such as having an African, African-Caribbean or south Asian background. Other people may be able to make adequate vitamin D from sunlight exposure from April to September. The NHS and Public Health England recommend that everyone, including those who are pregnant and breastfeeding, consider taking a daily supplement containing 10 μg (400 IU) of vitamin D during autumn and winter because of inadequate sunlight for vitamin D synthesis.[121]
United States
The dietary reference intake for vitamin D issued in 2010 by the Institute of Medicine (IoM) (renamed National Academy of Medicine in 2015), superseded previous recommendations which were expressed in terms of adequate intake. The recommendations were formed assuming the individual has no skin synthesis of vitamin D because of inadequate sun exposure. The reference intake for vitamin D refers to total intake from food, beverages and supplements, and assumes that calcium requirements are being met.[59]:5 The tolerable upper intake level (UL)[122] is defined as "the highest average daily intake of a nutrient that is likely to pose no risk of adverse health effects for nearly all persons in the general population."[59]:403 Although ULs are believed to be safe, information on the long-term effects is incomplete and these levels of intake are not recommended for long-term consumption.[59]:403:433
For US food and dietary supplement labeling purposes, the amount in a serving is expressed as a percent of Daily Value (%DV). For vitamin D labeling purposes, 100% of the daily value was 400 IU (10 μg), but in May 2016, it was revised to 800 IU (20 μg) to bring it into agreement with the recommended dietary allowance (RDA).[123][124] Compliance with the updated labeling regulations was required by 1 January 2020 for manufacturers with US$10 million or more in annual food sales, and by 1 January 2021 for manufacturers with lower volume food sales.[73][125] A table of the old and new adult daily values is provided at Reference Daily Intake.
Canada
Health Canada published recommended dietary intakes (DRIs) and tolerable upper intake levels (ULs) for vitamin D based on the jointly commissioned and funded Institute of Medicine 2010 report.[59][117]
Australia and New Zealand
Australia and New Zealand published nutrient reference values including guidelines for dietary vitamin D intake in 2006.[115] About a third of Australians have vitamin D deficiency.[126][127]
European Union
The European Food Safety Authority (EFSA) in 2016[118] reviewed the current evidence, finding the relationship between serum 25(OH)D concentration and musculoskeletal health outcomes is widely variable. They considered that average requirements and population reference intakes values for vitamin D cannot be derived, and that a serum 25(OH)D concentration of 50 nmol/L was a suitable target value. For all people over the age of 1, including women who are pregnant or lactating, they set an adequate intake of 15 μg/day (600 IU).[118]
The EFSA reviewed safe levels of intake in 2012,[119] setting the tolerable upper limit for adults at 100 μg/day (4000 IU), a similar conclusion as the IOM.
The Swedish National Food Agency recommends a daily intake of 10 μg (400 IU) of vitamin D3 for children and adults up to 75 years, and 20 μg (800 IU) for adults 75 and older.[128]
Non-government organisations in Europe have made their own recommendations. The German Society for Nutrition recommends 20 μg.[129] The European Menopause and Andropause Society recommends postmenopausal women consume 15 μg (600 IU) until age 70, and 20 μg (800 IU) from age 71. This dose should be increased to 100 μg (4,000 IU) in some patients with very low vitamin D status or in case of co-morbid conditions.[130]
Sources
Although vitamin D is present naturally in only a few foods,[2] it is commonly added as a fortification in manufactured foods. In some countries, staple foods are artificially fortified with vitamin D.[131]
Natural sources
| Animal sources | |||
| Source[132] | IU/g | Irregular | |
|---|---|---|---|
| Cooked egg yolk | 0.7 | 44 IU for a 61g egg | |
| Beef liver, cooked, braised | 0.5 | ||
| Fish liver oils, such as cod liver oil | 100 | 450 IU per teaspoon (4.5 g) | |
| Fatty fish species | |||
| Salmon, pink, cooked, dry heat | 5.2 | ||
| Mackerel, Pacific and jack, mixed species, cooked, dry heat | 4.6 | ||
| Tuna, canned in oil | 2.7 | ||
| Sardines, canned in oil, drained | 1.9 | ||
| Fungal sources | |||
| Source | μg/g | IU/g | |
|---|---|---|---|
| Cladonia arbuscula (lichen), thalli, dry[133] | vitamin D3 | 0.67–2.04 | 27–82 |
| vitamin D2 | 0.22–0.55 | 8.8–22 | |
| Agaricus bisporus (common mushroom): D2 + D3 | |||
| Portobello | Raw | 0.003 | 0.1 |
| Exposed to ultraviolet light | 0.11 | 4.46 | |
| Crimini | Raw | 0.001 | 0.03 |
| Exposed to ultraviolet light | 0.32 | 12.8 | |
In general, vitamin D3 is found in animal source foods, particularly fish, meat, offal, egg and dairy.[134] Vitamin D2 is found in fungi and is produced by ultraviolet irradiation of ergosterol.[135] The vitamin D2 content in mushrooms and Cladina arbuscula, a lichen, increases with exposure to ultraviolet light,[133][136] and is stimulated by industrial ultraviolet lamps for fortification.[135] The United States Department of Agriculture reports D2 and D3 content combined in one value.
Food fortification
Manufactured foods fortified with vitamin D include some fruit juices and fruit juice drinks, meal replacement energy bars, soy protein-based beverages, certain cheese and cheese products, flour products, infant formulas, many breakfast cereals, and milk.[137][138]
In 2016 in the United States, the Food and Drug Administration (FDA) amended food additive regulations for milk fortification,[139] stating that vitamin D3 levels not exceed 42 IU vitamin D per 100 g (400 IU per US quart) of dairy milk, 84 IU of vitamin D2 per 100 g (800 IU per quart) of plant milks, and 89 IU per 100 g (800 IU per quart) in plant-based yogurts or in soy beverage products.[140][141][142] Plant milks are defined as beverages made from soy, almond, rice, among other plant sources intended as alternatives to dairy milk.[143]
While some studies have found that vitamin D3 raises 25(OH)D blood levels faster and remains active in the body longer,[144][145] others contend that vitamin D2 sources are equally bioavailable and effective as D3 for raising and sustaining 25(OH)D.[135][146][147]
Food preparation
Vitamin D content in typical foods is reduced variably by cooking. Boiled, fried and baked foods retained 69–89% of original vitamin D.[148]
Recommended serum levels
Recommendations on recommended 25(OH)D serum levels vary across authorities, and vary based on factors like age.[2] US labs generally report 25(OH)D levels in ng/mL.[151] Other countries often use nmol/L.[151] One ng/mL is approximately equal to 2.5 nmol/L.[152]
A 2014 review concluded that the most advantageous serum levels for 25(OH)D for all outcomes appeared to be close to 30 ng/mL (75 nmol/L).[153] The optimal vitamin D levels are still controversial and another review concluded that ranges from 30 to 40 ng/mL (75 to 100 nmol/L) were to be recommended for athletes.[154] Part of the controversy is because numerous studies have found differences in serum levels of 25(OH)D between ethnic groups; studies point to genetic as well as environmental reasons behind these variations.[155] Supplementation to achieve these standard levels could cause harmful vascular calcification.[34]
A 2012 meta-analysis showed that the risk of cardiovascular diseases increases when blood levels of vitamin D are lowest in a range of 8 to 24 ng/mL (20 to 60 nmol/L), although results among the studies analyzed were inconsistent.[156]
In 2011 an IOM committee concluded a serum 25(OH)D level of 20 ng/mL (50 nmol/L) is needed for bone and overall health. The dietary reference intakes for vitamin D are chosen with a margin of safety and 'overshoot' the targeted serum value to ensure the specified levels of intake achieve the desired serum 25(OH)D levels in almost all persons. No contributions to serum 25(OH)D level are assumed from sun exposure and the recommendations are fully applicable to people with dark skin or negligible exposure to sunlight. The Institute found serum 25(OH)D concentrations above 30 ng/mL (75 nmol/L) are "not consistently associated with increased benefit". Serum 25(OH)D levels above 50 ng/mL (125 nmol/L) may be cause for concern. However, some people with serum 25(OH)D between 30 and 50 ng/mL (75 nmol/L-125 nmol/L) will also have inadequate vitamin D.[59]
Excess
Vitamin D toxicity is rare.[25] It is caused by supplementing with high doses of vitamin D rather than sunlight. The threshold for vitamin D toxicity has not been established; however, according to some research, the tolerable upper intake level (UL) is 4,000 IU/day for ages 9–71[157] (100 μg/day), while other research concludes that, in healthy adults, sustained intake of more than 50,000 IU/day (1250 μg) can produce overt toxicity after several months and can increase serum 25-hydroxyvitamin D levels to 150 ng/mL and greater.[25][158] Those with certain medical conditions, such as primary hyperparathyroidism,[159] are far more sensitive to vitamin D and develop hypercalcemia in response to any increase in vitamin D nutrition, while maternal hypercalcemia during pregnancy may increase fetal sensitivity to effects of vitamin D and lead to a syndrome of intellectual disability and facial deformities.[159][160]
Idiopathic infantile hypercalcemia is caused by a mutation of the CYP24A1 gene, leading to a reduction in the degradation of vitamin D. Infants who have such a mutation have an increased sensitivity to vitamin D and in case of additional intake a risk of hypercalcaemia.[161][162] The disorder can continue into adulthood.[163]
A review published in 2015 noted that adverse effects have been reported only at 25(OH)D serum concentrations above 200 nmol/L.[154]
Published cases of toxicity involving hypercalcemia in which the vitamin D dose and the 25-hydroxy-vitamin D levels are known all involve an intake of ≥40,000 IU (1,000 μg) per day.[159]
Those who are pregnant or breastfeeding should consult a doctor before taking a vitamin D supplement. The FDA advised manufacturers of liquid vitamin D supplements that droppers accompanying these products should be clearly and accurately marked for 400 international units (1 IU is the biological equivalent of 25 ng cholecalciferol/ergocalciferol). In addition, for products intended for infants, the FDA recommends the dropper hold no more than 400 IU.[164] For infants (birth to 12 months), the tolerable upper limit (maximum amount that can be tolerated without harm) is set at 25 μg/day (1,000 IU). One thousand micrograms per day in infants has produced toxicity within one month.[158] After being commissioned by the Canadian and American governments, the Institute of Medicine (IOM) (As of November 2010), has increased the tolerable upper limit (UL) to 2,500 IU per day for ages 1–3 years, 3,000 IU per day for ages 4–8 years and 4,000 IU per day for ages 9–71+ years (including pregnant or lactating women).[157]
Calcitriol itself is auto-regulated in a negative feedback cycle, and is also affected by parathyroid hormone, fibroblast growth factor 23, cytokines, calcium, and phosphate.[165]
A study published in 2017 assessed the prevalence of high daily intake levels of supplemental vitamin D among adults ages 20+ in the United States, based on publicly available NHANES data from 1999 through 2014. Its data shows the following:
- Over 18% of the population exceeds the NIH daily recommended allowance (RDA) of 600–800 IU,[2] by taking over 1000 IU, which suggests intentional supplement intake.[166]
- Over 3% of the population exceeds the NIH daily tolerable upper intake level (UL) of 4000 IU,[2] above which level the risk of toxic effects increases.[167][166]
- The percentage of the population taking over 1000 IU/day, as well as the percentage taking over 4000 IU/day, have both increased since 1999, according to trend analysis.[166]
Effect of excess
Vitamin D overdose causes hypercalcemia, which is a strong indication of vitamin D toxicity – this can be noted with an increase in urination and thirst. If hypercalcemia is not treated, it results in excess deposits of calcium in soft tissues and organs such as the kidneys, liver, and heart, resulting in pain and organ damage.[25][30][168]
The main symptoms of vitamin D overdose are hypercalcemia including anorexia, nausea, and vomiting. These may be followed by polyuria, polydipsia, weakness, insomnia, nervousness, pruritus and ultimately kidney failure. Furthermore, proteinuria, urinary casts, azotemia, and metastatic calcification (especially in the kidneys) may develop.[158] Other symptoms of vitamin D toxicity include intellectual disability in young children, abnormal bone growth and formation, diarrhea, irritability, weight loss, and severe depression.[25][168]
Vitamin D toxicity is treated by discontinuing vitamin D supplementation and restricting calcium intake. Kidney damage may be irreversible. Exposure to sunlight for extended periods of time does not normally cause vitamin D toxicity. The concentrations of vitamin D precursors produced in the skin reach an equilibrium, and any further vitamin D produced is degraded.[159]
Biosynthesis
Synthesis of vitamin D in nature is dependent on the presence of UV radiation and subsequent activation in the liver and in the kidneys. Many animals synthesize vitamin D3 from 7-dehydrocholesterol, and many fungi synthesize vitamin D2 from ergosterol.[135][169]
Interactive pathway
Click on icon in lower right corner to open.
Photochemistry
The transformation that converts 7-dehydrocholesterol to vitamin D3 occurs in two steps.[170][171] First, 7-dehydrocholesterol is photolyzed by ultraviolet light in a 6-electron conrotatory ring-opening electrocyclic reaction; the product is previtamin D3. Second, previtamin D3 spontaneously isomerizes to vitamin D3 (cholecalciferol) in an antarafacial sigmatropic [1,7] hydride shift. At room temperature, the transformation of previtamin D3 to vitamin D3 in an organic solvent takes about 12 days to complete. The conversion of previtamin D3 to vitamin D3 in the skin is about 10 times faster than in an organic solvent.[172]
The conversion from ergosterol to vitamin D2 follows a similar procedure, forming previtamin D2 by photolysis, which isomerizes to vitamin D2 (ergocalciferol).[173] The transformation of previtamin D2 to vitamin D2 in methanol has a rate comparable to that of previtamin D3. The process is faster in white button mushrooms.[135](fig. 3)
Synthesis in the skin
Vitamin D3 is produced photochemically from 7-dehydrocholesterol in the skin of most vertebrate animals, including humans.[174] The precursor of vitamin D3, 7-dehydrocholesterol is produced in relatively large quantities. 7-Dehydrocholesterol reacts with UVB light at wavelengths of 290–315 nm.[175] These wavelengths are present in sunlight, as well as in the light emitted by the UV lamps in tanning beds (which produce ultraviolet primarily in the UVA spectrum, but typically produce 4% to 10% of the total UV emissions as UVB, some tanning beds can use only separate UVB light bulbs specifically for vitamin D production). Exposure to light through windows is insufficient because glass almost completely blocks UVB light.[176]
Adequate amounts of vitamin D can be produced with moderate sun exposure to the face, arms and legs (for those with the least melanin), averaging 5–30 minutes twice per week, or approximately 25% of the time for minimal sunburn. The darker the skin on the Fitzpatrick scale and the weaker the sunlight, the more minutes of exposure are needed. It also depends on parts of body exposed, all three factors affect minimal erythema dose (MED).[177] Vitamin D overdose from UV exposure is impossible: the skin reaches an equilibrium where the vitamin D degrades as fast as it is created.[25][178]
The skin consists of two primary layers: the inner layer called the dermis, and the outer, thinner epidermis. Vitamin D is produced in the keratinocytes of two innermost strata of the epidermis, the stratum basale and stratum spinosum, which also are able to produce calcitriol and express the VDR.[179]
Evolution
Vitamin D can be synthesized only by a photochemical process. Its production from sterols would have started very early in the evolution of life around the origin of photosynthesis, possibly helping to prevent DNA damage by absorbing UVB, making vitamin D an inactive end product. The familiar vitamin D endocrine machinery containing vitamin D receptor (VDR), various CYP450 enzymes for activation and inactivation, and a vitamin D binding protein (DBP) is found in vertebrates only. Primitive marine vertebrates are thought to absorb calcium from the ocean into their skeletons and eat plankton rich in vitamin D, although the function in those without a calcified cartilage is unclear.[180] Phytoplankton in the ocean (such as coccolithophore and Emiliania huxleyi) have been photosynthesizing vitamin D for more than 500 million years.
Land vertebrates required another source of vitamin D other than plants for their calcified skeletons. They had to either ingest it or be exposed to sunlight to photosynthesize it in their skin.[169][172] Land vertebrates have been photosynthesizing vitamin D for more than 350 million years.[181]
In birds and fur-bearing mammals, fur or feathers block UV rays from reaching the skin. Instead, vitamin D is created from oily secretions of the skin deposited onto the feathers or fur, and is obtained orally during grooming.[182] However, some animals, such as the naked mole-rat, are naturally cholecalciferol-deficient, as serum 25-OH vitamin D levels are undetectable.[183] Dogs and cats are practically incapable of vitamin D synthesis due to high activity of 7-dehydrocholesterol reductase, but get vitamin D from prey animals.[184]
Industrial synthesis
Vitamin D3 (cholecalciferol) is produced industrially by exposing 7-dehydrocholesterol to UVB and UVC light, followed by purification.[185][135] The 7-dehydrocholesterol is a natural substance in fish organs, especially the liver,[186] in wool grease (lanolin) from sheep and in some plants, like lichen (Cladonia rangiferina).[187][188] Vitamin D2 (ergocalciferol) is produced in a similar way using ergosterol from yeast or mushrooms as a starting material.[185][135]
Mechanism of action
Metabolic activation
Vitamin D is carried via the blood to the liver, where it is converted into the prohormone calcifediol. Circulating calcifediol may then be converted into calcitriol – the biologically active form of vitamin D – in the kidneys.[189]
Whether synthesized in the skin or ingested, vitamin D is hydroxylated in the liver at position 25 (upper right of the molecule) to form 25-hydroxycholecalciferol (calcifediol or 25(OH)D).[4] This reaction is catalyzed by the microsomal enzyme vitamin D 25-hydroxylase, the product of the CYP2R1 human gene, and expressed by hepatocytes.[190] Once made, the product is released into the plasma, where it is bound to an α-globulin carrier protein named the vitamin D-binding protein.[191]
Calcifediol is transported to the proximal tubules of the kidneys, where it is hydroxylated at the 1-α position (lower right of the molecule) to form calcitriol (1,25-dihydroxycholecalciferol, 1,25(OH)2D).[1] The conversion of calcifediol to calcitriol is catalyzed by the enzyme 25-hydroxyvitamin D3 1-alpha-hydroxylase, which is the product of the CYP27B1 human gene.[1] The activity of CYP27B1 is increased by parathyroid hormone, and also by low calcium or phosphate.[1] Following the final converting step in the kidney, calcitriol is released into the circulation. By binding to vitamin D-binding protein, calcitriol is transported throughout the body, including to the intestine, kidneys, and bones.[17] Calcitriol is the most potent natural ligand of the vitamin D receptor, which mediates most of the physiological actions of vitamin D.[1][189] In addition to the kidneys, calcitriol is also synthesized by certain other cells, including monocyte-macrophages in the immune system. When synthesized by monocyte-macrophages, calcitriol acts locally as a cytokine, modulating body defenses against microbial invaders by stimulating the innate immune system.[189]
Inactivation
The activity of calcifediol and calcitriol can be reduced by hydroxylation at position 24 by vitamin D3 24-hydroxylase, forming secalciferol and calcitetrol, respectively.[4]
Difference between substrates
Vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol) share a similar mechanism of action as outlined above.[4] Metabolites produced by vitamin D2 are named with an er- or ergo- prefix to differentiate them from the D3-based counterparts (sometimes with a chole- prefix).[16]
- Metabolites produced from vitamin D2 tend to bind less well to the vitamin D-binding protein.[4]
- Vitamin D3 can alternatively be hydroxylated to calcifediol by sterol 27-hydroxylase (CYP27A1), but vitamin D2 cannot.[4]
- Ergocalciferol can be directly hydroxylated at position 24 by CYP27A1.[4] This hydroxylation also leads to a greater degree of inactivation: the activity of calcitriol decreases to 60% of original after 24-hydroxylation,[192] whereas ercalcitriol undergoes a 10-fold decrease in activity on conversion to ercalcitetrol.[193]
It is disputed whether these differences lead to a measurable drop in efficacy (see § Food fortification).
Intracellular mechanisms
Calcitriol enters the target cell and binds to the vitamin D receptor in the cytoplasm. This activated receptor enters the nucleus and binds to vitamin D response elements (VDRE) which are specific DNA sequences on genes.[1] Transcription of these genes is stimulated and produces greater levels of the proteins which mediate the effects of vitamin D.[4]
Some reactions of the cell to calcitriol appear to be too fast for the classical VDRE transcription pathway, leading to the discovery of various non-genomic actions of vitamin D. The membrane-bound PDIA3 likely serves as an alternate receptor in this pathway.[194] The classical VDR may still play a role.[195]
History
Vitamin D was discovered in 1922 following on from previous research.[196] American researchers Elmer McCollum and Marguerite Davis in 1914[11] discovered a substance in cod liver oil which later was called "vitamin A". British doctor Edward Mellanby noticed dogs that were fed cod liver oil did not develop rickets and concluded vitamin A, or a closely associated factor, could prevent the disease. In 1922, Elmer McCollum tested modified cod liver oil in which the vitamin A had been destroyed.[11] The modified oil cured the sick dogs, so McCollum concluded the factor in cod liver oil which cured rickets was distinct from vitamin A. He called it vitamin D because he thought it was the fourth vitamin to be named.[197][198] It was not initially realized that vitamin D can be synthesized by humans (in the skin) through exposure to UV light, and therefore is technically not a vitamin, but rather can be considered to be a hormone.
In 1925,[11] it was established that when 7-dehydrocholesterol is irradiated with light, a form of a fat-soluble substance is produced (now known as D3). Alfred Fabian Hess stated: "Light equals vitamin D."[199] Adolf Windaus, at the University of Göttingen in Germany, received the Nobel Prize in Chemistry in 1928 for his work on the constitution of sterols and their connection with vitamins.[200] In 1929, a group at NIMR in Hampstead, London, were working on the structure of vitamin D, which was still unknown, as well as the structure of steroids. A meeting took place with J.B.S. Haldane, J.D. Bernal, and Dorothy Crowfoot to discuss possible structures, which contributed to bringing a team together. X-ray crystallography demonstrated the sterol molecules were flat, not as proposed by the German team led by Windaus. In 1932, Otto Rosenheim and Harold King published a paper putting forward structures for sterols and bile acids which found immediate acceptance.[201] The informal academic collaboration between the team members Robert Benedict Bourdillon, Otto Rosenheim, Harold King, and Kenneth Callow was very productive and led to the isolation and characterization of vitamin D.[202] At this time, the policy of the Medical Research Council was not to patent discoveries, believing the results of medical research should be open to everybody. In the 1930s, Windaus clarified further the chemical structure of vitamin D.[203]
In 1923, American biochemist Harry Steenbock at the University of Wisconsin demonstrated that irradiation by ultraviolet light increased the vitamin D content of foods and other organic materials.[204] After irradiating rodent food, Steenbock discovered the rodents were cured of rickets. Using US$300 of his own money, Steenbock patented his invention. His irradiation technique was used for foodstuffs, most notably for milk. By the expiration of his patent in 1945, rickets had been all but eliminated in the US.[205]
In 1969, a specific binding protein for vitamin D called the vitamin D receptor was identified.[206] Shortly thereafter, the conversion of vitamin D to calcifediol and then to calcitriol, the biologically active form, was confirmed.[9][10][207] The photosynthesis of vitamin D3 in skin via previtamin D3 and its subsequent metabolism was described in 1980.[208]
Research
There is conflicting evidence about the benefits of interventions with vitamin D. Supplementation of between 800 and 1,000 IU is safe, but higher levels leading to blood levels of more than 50 ng/mL (125 nmol/L) may cause adverse effects.[2][209]
The US Office of Dietary Supplements established a Vitamin D Initiative over 2004–18 to track current research and provide education to consumers.[210] As of 2022, the role of vitamin D in the prevention and treatment of diabetes, glucose intolerance, hypertension, multiple sclerosis, and other medical conditions remains under preliminary research.[2]
Some preliminary studies link low vitamin D levels with disease later in life.[211] One meta-analysis found a decrease in mortality in elderly people.[12] Another meta-analysis covering over 350,000 people concluded that vitamin D supplementation in unselected community-dwelling individuals does not reduce skeletal (total fracture) or non-skeletal outcomes (myocardial infarction, ischemic heart disease, stroke, cerebrovascular disease, cancer) by more than 15%, and that further research trials with similar design are unlikely to change these conclusions.[14] As of 2022, there is insufficient evidence for an effect of vitamin D supplementation on the risk of cancer.[2][212][213] A 2019 meta-analysis found a small increase in risk of stroke when calcium and vitamin D supplements were taken together.[214]
COVID-19
(As of September 2022) the US National Institutes of Health state there is insufficient evidence to recommend for or against using vitamin D supplementation to prevent or treat COVID-19.[215] The UK National Institute for Health and Care Excellence (NICE) does not recommend to offer a vitamin D supplement to people solely to prevent or treat COVID-19.[216][217] Both organizations included recommendations to continue the previous established recommendations on vitamin D supplementation for other reasons, such as bone and muscle health, as applicable. Both organizations noted that more people may require supplementation due to lower amounts of sun exposure during the pandemic.[215][216]
Several systematic reviews and meta-analyses of multiple studies have described the associations of vitamin D deficiency with adverse outcomes in COVID-19.[218][219][220][221][222][223] In the largest analysis, with data from 76 observational studies including almost two million adults, vitamin D deficiency or insufficiency significantly increased the susceptibility to becoming infected with COVID-19 and having severe COVID-19, with odds ratios of 1.5 and 1.9 respectively, but these findings had high risk of bias and heterogeneity. A two-fold greater mortality was found, but this analysis was less robust.[223] These findings confirm smaller, earlier analyses,[219][220][221][222] one of which, in reporting that people with COVID-19 tend to have lower 25(OH)D levels than healthy subjects, stated that the trend for associations with health outcomes was limited by the low quality of the studies and by the possibility of reverse causality mechanisms.[221]
A meta-analysis of three studies on the effect of oral vitamin D or calcifediol supplementation indicated a lower intensive care unit (ICU) admission rate (odds ratio: 0.36) compared to those without supplementation, but without a change in mortality.[224] A Cochrane review, also of three studies, found the evidence for the effectiveness of vitamin D supplementation for the treatment of COVID-19 to be very uncertain.[225] They found there was substantial clinical and methodological heterogeneity in the three studies that were included, mainly because of different supplementation strategies, vitamin D formulations (one using calcifediol), pre-treatment status and reported outcomes.[225] Another meta-analysis stated that the use of high doses of vitamin D in people with COVID-19 is not based on solid evidence although calcifediol supplementation may have a protective effect on ICU admissions.[221]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 "Vitamin D". Micronutrient Information Center, Linus Pauling Institute, Oregon State University, Corvallis. 11 February 2021. https://lpi.oregonstate.edu/mic/vitamins/vitamin-D.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 "Vitamin D". Office of Dietary Supplements, US National Institutes of Health. 12 August 2022. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/.
- ↑ 3.0 3.1 3.2 3.3 "From vitamin D to hormone D: fundamentals of the vitamin D endocrine system essential for good health". The American Journal of Clinical Nutrition 88 (2): 491S–9S. August 2008. doi:10.1093/ajcn/88.2.491S. PMID 18689389.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 "Vitamin D metabolism, mechanism of action, and clinical applications". Chemistry & Biology 21 (3): 319–29. March 2014. doi:10.1016/j.chembiol.2013.12.016. PMID 24529992.
- ↑ "Efficacy of fish intake on vitamin D status: a meta-analysis of randomized controlled trials". The American Journal of Clinical Nutrition 102 (4): 837–47. October 2015. doi:10.3945/ajcn.114.105395. PMID 26354531.
- ↑ Cardwell, Glenn et al. “A Review of Mushrooms as a Potential Source of Dietary Vitamin D.” Nutrients vol. 10,10 1498. 13 Oct. 2018, doi:10.3390/nu10101498
- ↑ "Vitamin D Tests". Lab Tests Online (USA). American Association for Clinical Chemistry. http://labtestsonline.org/understanding/analytes/vitamin-d/tab/sample.
- ↑ "Assessment of vitamin D nutritional and hormonal status: what to measure and how to do it". Calcified Tissue International 58 (1): 4–5. January 1996. doi:10.1007/BF02509538. PMID 8825231.
- ↑ 9.0 9.1 "Identification of 1,25-dihydroxycholecalciferol, a form of vitamin D3 metabolically active in the intestine". Proceedings of the National Academy of Sciences of the United States of America 68 (4): 803–4. April 1971. doi:10.1073/pnas.68.4.803. PMID 4323790. Bibcode: 1971PNAS...68..803H.
- ↑ 10.0 10.1 "1,25-dihydroxycholecalciferol: identification of the proposed active form of vitamin D3 in the intestine". Science 173 (3991): 51–4. July 1971. doi:10.1126/science.173.3991.51. PMID 4325863. Bibcode: 1971Sci...173...51N.
- ↑ 11.0 11.1 11.2 11.3 "The discovery of vitamin D: the contribution of Adolf Windaus". The Journal of Nutrition 134 (6): 1299–302. June 2004. doi:10.1093/jn/134.6.1299. PMID 15173387.
- ↑ 12.0 12.1 12.2 12.3 "Vitamin D supplementation for prevention of mortality in adults". The Cochrane Database of Systematic Reviews 1 (1): CD007470. January 2014. doi:10.1002/14651858.CD007470.pub3. PMID 24414552.
- ↑ 13.0 13.1 "Effects of vitamin D supplements on bone mineral density: a systematic review and meta-analysis". Lancet 383 (9912): 146–55. January 2014. doi:10.1016/s0140-6736(13)61647-5. PMID 24119980.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 "The effect of vitamin D supplementation on skeletal, vascular, or cancer outcomes: a trial sequential meta-analysis". The Lancet. Diabetes & Endocrinology 2 (4): 307–20. April 2014. doi:10.1016/S2213-8587(13)70212-2. PMID 24703049.
- ↑ "The Lancet Diabetes & Endocrinology: Vitamin D supplementation in adults does not prevent fractures, falls or improve bone mineral density". https://www.eurekalert.org/news-releases/808633. "The authors conclude that there is therefore little reason to use vitamin D supplements to maintain or improve musculoskeletal health, except for the prevention of rare conditions such as rickets and osteomalacia in high risk groups, which can be caused by vitamin D deficiency after long lack of exposure to sunshine."
- ↑ 16.0 16.1 "IUPAC-IUB Joint Commission on Biochemical Nomenclature (JCBN): Nomenclature of vitamin D. Recommendations 1981". European Journal of Biochemistry 124 (2): 223–7. May 1982. doi:10.1111/j.1432-1033.1982.tb06581.x. PMID 7094913.
- ↑ 17.0 17.1 17.2 BP Marriott, ed (2020). "Vitamin D". Present Knowledge in Nutrition, Eleventh Edition. London, United Kingdom: Academic Press (Elsevier). pp. 93–114. ISBN 978-0-323-66162-1.
- ↑ Medical Physiology E-Book. Elsevier Health Sciences. 29 March 2016. ISBN 978-1-4557-3328-6. https://books.google.com/books?id=6QzhCwAAQBAJ. Retrieved 9 April 2017.
- ↑ "Intestinal calcium absorption: Molecular vitamin D mediated mechanisms". Journal of Cellular Biochemistry 88 (2): 332–9. February 2003. doi:10.1002/jcb.10360. PMID 12520535.
- ↑ 20.0 20.1 20.2 "Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease". The American Journal of Clinical Nutrition 80 (6 Suppl): 1678S–88S. December 2004. doi:10.1093/ajcn/80.6.1678S. PMID 15585788.
- ↑ 21.0 21.1 "The biology and pathology of vitamin D control in bone". Journal of Cellular Biochemistry 111 (1): 7–13. September 2010. doi:10.1002/jcb.22661. PMID 20506379.
- ↑ "An update on the association of vitamin D deficiency with common infectious diseases". Canadian Journal of Physiology and Pharmacology 93 (5): 363–8. May 2015. doi:10.1139/cjpp-2014-0352. PMID 25741906.
- ↑ "Vitamin D increases expression of the tyrosine hydroxylase gene in adrenal medullary cells". Brain Research. Molecular Brain Research 36 (1): 193–6. February 1996. doi:10.1016/0169-328X(95)00314-I. PMID 9011759.
- ↑ 24.0 24.1 24.2 "Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline". The Journal of Clinical Endocrinology and Metabolism 96 (7): 1911–30. July 2011. doi:10.1210/jc.2011-0385. PMID 21646368.
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 25.6 "Vitamin D deficiency". The New England Journal of Medicine 357 (3): 266–81. July 2007. doi:10.1056/NEJMra070553. PMID 17634462.
- ↑ "Vitamin D deficiency in Europe: pandemic?". The American Journal of Clinical Nutrition 103 (4): 1033–44. April 2016. doi:10.3945/ajcn.115.120873. PMID 26864360.
- ↑ "Rickets". National Health Service. 8 March 2012. http://www.nhs.uk/conditions/Rickets/Pages/Introduction.aspx.
- ↑ "Global Consensus Recommendations on Prevention and Management of Nutritional Rickets". The Journal of Clinical Endocrinology and Metabolism 101 (2): 394–415. February 2016. doi:10.1210/jc.2015-2175. PMID 26745253.
- ↑ "Vitamin D deficiency and aging: implications for general health and osteoporosis". Biogerontology 3 (1–2): 73–7. 2002. doi:10.1023/A:1015263514765. PMID 12014847.
- ↑ 30.0 30.1 30.2 30.3 Nutrition Through the Life Cycle. Cengage Learning. 28 June 2013. ISBN 978-1-285-82025-5. https://books.google.com/books?id=TeQZBQAAQBAJ. Retrieved 9 April 2017.
- ↑ "Abundant sunshine and vitamin D deficiency". The British Journal of Nutrition 99 (6): 1171–3. June 2008. doi:10.1017/S0007114508898662. PMID 18234141.
- ↑ "Special considerations for vitamin D in the south Asian population in the UK". Therapeutic Advances in Musculoskeletal Disease 9 (6): 137–44. June 2017. doi:10.1177/1759720X17704430. PMID 28620422.
- ↑ "The uncertain significance of low vitamin D levels in African descent populations: a review of the bone and cardiometabolic literature". Progress in Cardiovascular Diseases 56 (3): 261–9. 2013. doi:10.1016/j.pcad.2013.10.015. PMID 24267433.
- ↑ 34.0 34.1 "Effect of race and genetics on vitamin D metabolism, bone and vascular health". Nature Reviews. Nephrology 8 (8): 459–66. June 2012. doi:10.1038/nrneph.2012.112. PMID 22688752.
- ↑ "Utility of sun-reactive skin typing and melanin index for discerning vitamin D deficiency". Pediatric Research 82 (3): 444–51. September 2017. doi:10.1038/pr.2017.114. PMID 28467404.
- ↑ 36.0 36.1 "Prevention of rickets and vitamin D deficiency in infants, children, and adolescents". Pediatrics 122 (5): 1142–52. November 2008. doi:10.1542/peds.2008-1862. PMID 18977996.
- ↑ "Interventions for the prevention of nutritional rickets in term born children". The Cochrane Database of Systematic Reviews 2010 (4): CD006164. October 2007. doi:10.1002/14651858.CD006164.pub2. PMID 17943890.
- ↑ "Pseudovitamin D deficiency rickets—a report from the Indian subcontinent". Postgraduate Medical Journal 76 (896): 369–72. June 2000. doi:10.1136/pmj.76.896.369. PMID 10824056.
- ↑ "The Return of Congenital Rickets, Are We Missing Occult Cases?". Calcified Tissue International 99 (3): 227–36. September 2016. doi:10.1007/s00223-016-0146-2. PMID 27245342.
- ↑ "Congenital rickets due to vitamin D deficiency in the mothers". Clinical Nutrition 34 (5): 793–8. October 2015. doi:10.1016/j.clnu.2014.12.006. PMID 25552383.
- ↑ "Adaptation of calcium absorption during treatment of nutritional rickets in Nigerian children". The British Journal of Nutrition 100 (2): 387–92. August 2008. doi:10.1017/S0007114507901233. PMID 18197991. https://espace.library.uq.edu.au/view/UQ:c3b1fb5/UQc3b1fb5_OA.pdf.
- ↑ "Nutritional rickets without vitamin D deficiency in Bangladesh". Journal of Tropical Pediatrics 45 (5): 291–3. October 1999. doi:10.1093/tropej/45.5.291. PMID 10584471.
- ↑ 43.0 43.1 "An epidemiological model of privational rickets and osteomalacia". The Proceedings of the Nutrition Society 56 (3): 939–56. November 1997. doi:10.1079/PNS19970100. PMID 9483661.
- ↑ "The role of cereals in the aetiology of nutritional rickets: the lesson of the Irish National Nutrition Survey 1943-8". The British Journal of Nutrition 45 (1): 17–22. January 1981. doi:10.1079/BJN19810073. PMID 6970590.
- ↑ "The problem of rickets in UK Asians". Journal of Human Nutrition and Dietetics 2 (2): 105–16. 1989. doi:10.1111/j.1365-277X.1989.tb00015.x.
- ↑ 46.0 46.1 "Nutritional rickets: deficiency of vitamin D, calcium, or both?". The American Journal of Clinical Nutrition 80 (6 Suppl): 1725S–9S. December 2004. doi:10.1093/ajcn/80.6.1725S. PMID 15585795.
- ↑ 47.0 47.1 "Meat consumption reduces the risk of nutritional rickets and osteomalacia". The British Journal of Nutrition 94 (6): 983–91. December 2005. doi:10.1079/BJN20051558. PMID 16351777.
- ↑ "A history of rickets in the United States". The American Journal of Clinical Nutrition 20 (11): 1234–41. November 1967. doi:10.1093/ajcn/20.11.1234. PMID 4862158.
- ↑ The Nutrition Desk Reference. McGraw-Hill. 1997. ISBN 978-0-87983-826-3. https://books.google.com/books?id=Z4hFKXI7EhsC. Retrieved 9 April 2017.
- ↑ Nature's Perfect Food: How Milk Became America's Drink. NYU Press. 1 February 2002. ISBN 978-0-8147-1938-1. https://books.google.com/books?id=Nr1_u2DvDckC. Retrieved 9 April 2017.
- ↑ "Previous milk consumption is associated with greater bone density in young women". The American Journal of Clinical Nutrition 69 (5): 1014–7. May 1999. doi:10.1093/ajcn/69.5.1014. PMID 10232644.
- ↑ "High prevalence of vitamin D inadequacy and implications for health". Mayo Clinic Proceedings 81 (3): 353–73. March 2006. doi:10.4065/81.3.353. PMID 16529140.
- ↑ "Vitamin D and chronic pain". Pain 141 (1–2): 10–3. January 2009. doi:10.1016/j.pain.2008.11.010. PMID 19084336.
- ↑ "Does vitamin D supplementation alleviate chronic nonspecific musculoskeletal pain? A systematic review and meta-analysis". Clinical Rheumatology 36 (5): 1201–08. May 2017. doi:10.1007/s10067-016-3205-1. PMID 26861032. https://www.researchgate.net/publication/293637550.
- ↑ "Vitamin D and calcium: a systematic review of health outcomes". Evidence Report/Technology Assessment (183): 1–420. August 2009. PMID 20629479.
- ↑ "Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials". BMJ 348: g2035. April 2014. doi:10.1136/bmj.g2035. PMID 24690624.
- ↑ 57.0 57.1 "Vitamin D status and ill health: a systematic review". The Lancet. Diabetes & Endocrinology 2 (1): 76–89. January 2014. doi:10.1016/S2213-8587(13)70165-7. PMID 24622671.
- ↑ "Vitamin D supplementation for the management of knee osteoarthritis: a systematic review of randomized controlled trials". Rheumatology International 37 (9): 1489–98. September 2017. doi:10.1007/s00296-017-3719-0. PMID 28421358.
- ↑ 59.00 59.01 59.02 59.03 59.04 59.05 59.06 59.07 59.08 59.09 59.10 Institute of Medicine (2011). "8, Implications and Special Concerns". Dietary Reference Intakes for Calcium and Vitamin D. The National Academies Collection: Reports funded by National Institutes of Health. National Academies Press. doi:10.17226/13050. ISBN 978-0-309-16394-1. https://www.ncbi.nlm.nih.gov/books/NBK56078/. Retrieved 17 September 2017.
- ↑ 60.0 60.1 "Nutrition advice: the vitamin D-lemma". Nature 475 (7354): 23–5. July 2011. doi:10.1038/475023a. PMID 21734684. http://www.nature.com/news/2011/110706/pdf/475023a.pdf. Retrieved 17 November 2011.
- ↑ "Vitamin D and mortality: meta-analysis of individual participant data from a large consortium of cohort studies from Europe and the United States". BMJ 348 (jun17 16): g3656. June 2014. doi:10.1136/bmj.g3656. PMID 24938302.
- ↑ "Vitamin D and aging". The Journal of Steroid Biochemistry and Molecular Biology 114 (1–2): 78–84. March 2009. doi:10.1016/j.jsbmb.2008.12.020. PMID 19444937.
- ↑ "Vitamin D, nervous system and aging". Psychoneuroendocrinology 34 (Suppl 1): S278–86. December 2009. doi:10.1016/j.psyneuen.2009.07.003. PMID 19660871.
- ↑ "Klotho protein deficiency and aging". Geriatrics & Gerontology International 10 (Suppl 1): S80-7. July 2010. doi:10.1111/j.1447-0594.2010.00596.x. PMID 20590845.
- ↑ "Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men". The Cochrane Database of Systematic Reviews 4 (4): CD000227. April 2014. doi:10.1002/14651858.CD000227.pub4. PMID 24729336.
- ↑ "A pooled analysis of vitamin D dose requirements for fracture prevention". The New England Journal of Medicine 367 (1): 40–9. July 2012. doi:10.1056/NEJMoa1109617. PMID 22762317. https://research.vu.nl/ws/files/709966/300335.pdf. Retrieved 17 July 2019.
- ↑ "Vitamin D with or without calcium supplementation for prevention of cancer and fractures: an updated meta-analysis for the U.S. Preventive Services Task Force". Annals of Internal Medicine 155 (12): 827–38. December 2011. doi:10.7326/0003-4819-155-12-201112200-00005. PMID 22184690.
- ↑ "Association Between Calcium or Vitamin D Supplementation and Fracture Incidence in Community-Dwelling Older Adults: A Systematic Review and Meta-analysis". JAMA 318 (24): 2466–2482. December 2017. doi:10.1001/jama.2017.19344. PMID 29279934.
- ↑ "Effectiveness and safety of vitamin D in relation to bone health". Evidence Report/Technology Assessment (158): 1–235. August 2007. PMID 18088161.
- ↑ "Vitamin D supplementation and falls: a trial sequential meta-analysis". The Lancet. Diabetes & Endocrinology 2 (7): 573–80. July 2014. doi:10.1016/S2213-8587(14)70068-3. PMID 24768505.
- ↑ "Sports health benefits of vitamin d". Sports Health 4 (6): 496–501. November 2012. doi:10.1177/1941738112461621. PMID 24179588.
- ↑ "Vitamin D, calcium or a combination of vitamin D and calcium for the treatment of nutritional rickets in children". The Cochrane Database of Systematic Reviews 2020 (4): CD012581. April 2020. doi:10.1002/14651858.CD012581.pub2. PMID 32303107.
- ↑ 73.0 73.1 "Changes to the Nutrition Facts Label". 27 May 2016. https://www.fda.gov/food/food-labeling-nutrition/changes-nutrition-facts-label.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Comparative efficacy of vitamin D status in reducing the risk of bladder cancer: A systematic review and network meta-analysis". Nutrition 32 (5): 515–523. May 2016. doi:10.1016/j.nut.2015.10.023. PMID 26822497.
- ↑ 75.0 75.1 "Circulating vitamin D levels and colorectal cancer risk: A meta-analysis and systematic review of case-control and prospective cohort studies". Critical Reviews in Food Science and Nutrition 63 (1): 1–17. July 2021. doi:10.1080/10408398.2021.1939649. PMID 34224246.
- ↑ 76.0 76.1 "Vitamin D and Clinical Cancer Outcomes: A Review of Meta-Analyses". JBMR Plus 5 (1): e10420. January 2021. doi:10.1002/jbm4.10420. PMID 33553987.
- ↑ "Vitamin D supplementation and total cancer incidence and mortality: a meta-analysis of randomized controlled trials". Annals of Oncology 30 (5): 733–743. May 2019. doi:10.1093/annonc/mdz059. PMID 30796437.
- ↑ "Vitamin D Supplementation and Cardiovascular Disease Risks in More Than 83 000 Individuals in 21 Randomized Clinical Trials: A Meta-analysis". JAMA Cardiology 4 (8): 765–76. August 2019. doi:10.1001/jamacardio.2019.1870. PMID 31215980.
- ↑ "Vitamin D supplementation, cardiac events and stroke: A systematic review and meta-regression analysis". Int J Cardiol Heart Vasc 28: 100537. 2020. doi:10.1016/j.ijcha.2020.100537. PMID 32462077.
- ↑ "Effect of Vitamin D Supplementation on Blood Pressure: A Systematic Review and Meta-analysis Incorporating Individual Patient Data". JAMA Internal Medicine 175 (5): 745–54. May 2015. doi:10.1001/jamainternmed.2015.0237. PMID 25775274.
- ↑ "Effect of Vitamin D on Blood Pressure and Hypertension in the General Population: An Update Meta-Analysis of Cohort Studies and Randomized Controlled Trials". Prev Chronic Dis 17: E03. 2020. doi:10.5888/pcd17.190307. PMID 31922371.
- ↑ "Vitamin D status and blood pressure in children and adolescents: a systematic review of observational studies". Systematic Reviews 10 (1): 60. 2021. doi:10.1186/s13643-021-01584-x. PMID 33618764.
- ↑ "Vitamin D and innate and adaptive immunity". Vitamins and the Immune System. Vitamins & Hormones. 86. Academic Press. 2011. pp. 23–62. doi:10.1016/B978-0-12-386960-9.00002-2. ISBN 9780123869609.
- ↑ "Vitamin D and immune regulation: antibacterial, antiviral, anti-inflammatory". JBMR Plus 5 (1): e10405. August 2020. doi:10.1002/jbm4.10405. PMID 32904944.
- ↑ "Low serum vitamin D levels and tuberculosis: a systematic review and meta-analysis". International Journal of Epidemiology 37 (1): 113–9. February 2008. doi:10.1093/ije/dym247. PMID 18245055.
- ↑ "Impact of vitamin D in the treatment of tuberculosis". The American Journal of the Medical Sciences 341 (6): 493–8. June 2011. doi:10.1097/MAJ.0b013e3182070f47. PMID 21289501.
- ↑ 87.0 87.1 "SACN rapid review: Vitamin D and acute respiratory tract infections". https://www.gov.uk/government/publications/sacn-rapid-review-vitamin-d-and-acute-respiratory-tract-infections.
- ↑ "Vitamin D to prevent exacerbations of COPD: systematic review and meta-analysis of individual participant data from randomised controlled trials". Thorax 74 (4): 337–345. April 2019. doi:10.1136/thoraxjnl-2018-212092. PMID 30630893.
- ↑ "Vitamin D for the management of asthma". Cochrane Database Syst Rev 2023 (2): CD011511. February 2023. doi:10.1002/14651858.CD011511.pub3. PMID 36744416.
- ↑ "Association Between Inflammatory Bowel Disease and Vitamin D Deficiency: A Systematic Review and Meta-analysis". Inflammatory Bowel Diseases 21 (11): 2708–2717. November 2015. doi:10.1097/MIB.0000000000000546. PMID 26348447.
- ↑ 91.0 91.1 91.2 91.3 91.4 "Vitamin D for the treatment of inflammatory bowel disease". The Cochrane Database of Systematic Reviews 2023 (10): CD011806. October 2023. doi:10.1002/14651858.CD011806.pub2. PMID 37781953.
- ↑ "Vitamin D Therapy in Adults With Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis". Inflammatory Bowel Diseases 26 (12): 1819–1830. May 2020. doi:10.1093/ibd/izaa087. PMID 32385487.
- ↑ "Effects of Vitamin D Supplementation on Prevention of Type 2 Diabetes in Patients With Prediabetes: A Systematic Review and Meta-analysis". Diabetes Care 43 (7): 1650–58. July 2020. doi:10.2337/dc19-1708. PMID 33534730.
- ↑ "The effects of vitamin D supplementation on indices of glycemic control in Iranian diabetics: A systematic review and meta-analysis". Complementary Therapies in Clinical Practice 34: 294–304. February 2019. doi:10.1016/j.ctcp.2018.12.009. PMID 30712741.
- ↑ "Serum vitamin D levels in relation to type-2 diabetes and prediabetes in adults: a systematic review and dose-response meta-analysis of epidemiologic studies". Critical Reviews in Food Science and Nutrition 2 (29): 8178–8198. June 2021. doi:10.1080/10408398.2021.1926220. PMID 34076544.
- ↑ "Interventions for latent autoimmune diabetes (LADA) in adults". The Cochrane Database of Systematic Reviews 2011 (9): CD006165. September 2011. doi:10.1002/14651858.cd006165.pub3. PMID 21901702.
- ↑ "Vitamin D Status and Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis of Observational Studies". Advances in Nutrition 9 (1): 9–20. January 2018. doi:10.1093/advances/nmx002. PMID 29438455.
- ↑ "The Effect of Vitamin D Supplementation on Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis of Randomized Controlled Trials". Journal of Child and Adolescent Psychopharmacology 29 (9): 670–87. November 2019. doi:10.1089/cap.2019.0059. PMID 31368773.
- ↑ "Vitamin D supplementation for depressive symptoms: a systematic review and meta-analysis of randomized controlled trials". Psychosomatic Medicine 76 (3): 190–6. April 2014. doi:10.1097/psy.0000000000000044. PMID 24632894.
- ↑ "Vitamin D, cognition, and dementia: a systematic review and meta-analysis". Neurology 79 (13): 1397–405. September 2012. doi:10.1212/WNL.0b013e31826c197f. PMID 23008220.
- ↑ "Correlation between total vitamin D levels and psychotic psychopathology in patients with schizophrenia: therapeutic implications for add-on vitamin D augmentation". Therapeutic Advances in Psychopharmacology 4 (6): 268–75. December 2014. doi:10.1177/2045125314553612. PMID 25489478.
- ↑ 102.0 102.1 "Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: systematic review and meta-analysis of observational studies". BMJ 346: f1169. March 2013. doi:10.1136/bmj.f1169. PMID 23533188.
- ↑ 103.0 103.1 "Vitamin D supplementation during pregnancy: Updated meta-analysis on maternal outcomes". The Journal of Steroid Biochemistry and Molecular Biology 164: 148–55. November 2016. doi:10.1016/j.jsbmb.2016.02.008. PMID 26877200.
- ↑ "Vitamin D supplementation during pregnancy: state of the evidence from a systematic review of randomised trials". BMJ 359: j5237. November 2017. doi:10.1136/bmj.j5237. PMID 29187358.
- ↑ 105.0 105.1 "Vitamin D supplementation for women during pregnancy". The Cochrane Database of Systematic Reviews 7 (7): CD008873. July 2019. doi:10.1002/14651858.CD008873.pub4. PMID 31348529.
- ↑ 106.0 106.1 "Vitamin D and its role during pregnancy in attaining optimal health of mother and fetus". Nutrients 4 (3): 208–30. March 2012. doi:10.3390/nu4030208. PMID 22666547.
- ↑ "Association Between Vitamin D Supplementation During Pregnancy and Offspring Growth, Morbidity, and Mortality: A Systematic Review and Meta-analysis". JAMA Pediatrics 172 (7): 635–45. July 2018. doi:10.1001/jamapediatrics.2018.0302. PMID 29813153.
- ↑ "Vitamin D supplementation and body weight status: a systematic review and meta-analysis of randomized controlled trials". Obesity Reviews 15 (6): 528–37. June 2014. doi:10.1111/obr.12162. PMID 24528624.
- ↑ "Vitamin D status and weight loss: a systematic review and meta-analysis of randomized and nonrandomized controlled weight-loss trials". The American Journal of Clinical Nutrition 104 (4): 1151–1159. October 2016. doi:10.3945/ajcn.116.136879. PMID 27604772.
- ↑ 110.0 110.1 110.2 ((European Food Safety Authority (EFSA) Panel on Dietetic Products, Nutrition and Allergies (NDA) )) (2010). "Scientific opinion on the substantiation of health claims related to vitamin D and normal function of the immune system and inflammatory response (ID 154, 159), maintenance of normal muscle function (ID 155) and maintenance of normal cardiovascular function (ID 159) pursuant to Article 13(1) of Regulation (EC) No 1924/2006". EFSA Journal 8 (2): 1468–85. doi:10.2903/j.efsa.2010.1468.
- ↑ ((European Food Safety Authority (EFSA) Panel on Dietetic Products, Nutrition and Allergies (NDA) )) (2011). "Scientific opinion on the substantiation of a health claim related to vitamin D and risk of falling pursuant to Article 14 of Regulation (EC) No 1924/2006". EFSA Journal 9 (9): 2382–2400. doi:10.2903/j.efsa.2011.2382. http://orbit.dtu.dk/files/6355745/prod11324398702885.Scientific.pdf. Retrieved 20 August 2019.
- ↑ "Guidance for Industry: Food Labeling Guide". Food and Drug Administration (FDA). January 2013. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-food-labeling-guide.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Health Canada Scientific Summary on the U. S. Health Claim Regarding Calcium and Osteoporosis". Bureau of Nutritional Sciences Food Directorate, Health Products and Food Branch Health Canada. 1 May 2000. http://www.hc-sc.gc.ca/fn-an/label-etiquet/claims-reclam/assess-evalu/calcium_osteo-eng.php.
- ↑ "Regulatory Systems of Health Claims in Japan". Japan Consumer Affairs Agency, Food Labelling Division. 1 June 2011. http://www.caa.go.jp/en/pdf/syokuhin338.pdf.
- ↑ 115.0 115.1 115.2 115.3 115.4 Nutrient Reference Values for Australia and New Zealand Including Recommended Dietary Intakes. Canberra: National Health and Medical Research Council. 2006. ISBN 1864962437. https://www.nhmrc.gov.au/about-us/publications/nutrient-reference-values-australia-and-new-zealand-including-recommended-dietary-intakes#block-views-block-file-attachments-content-block-1. Retrieved 19 March 2023.
- ↑ 116.0 116.1 116.2 116.3 "Vitamins and minerals – Vitamin D". 3 August 2020. http://www.nhs.uk/Conditions/vitamins-minerals/Pages/Vitamin-D.aspx.
- ↑ 117.0 117.1 117.2 117.3 "Vitamin D and Calcium: Updated Dietary Reference Intakes". Nutrition and Healthy Eating. Health Canada. 5 December 2008. https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/vitamins-minerals/vitamin-calcium-updated-dietary-reference-intakes-nutrition.html.
- ↑ 118.0 118.1 118.2 118.3 EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA) (29 June 2016). "Dietary reference values for vitamin D". EFSA Journal 14 (10): e04547. doi:10.2903/j.efsa.2016.4547.
- ↑ 119.0 119.1 EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA) (2012). "Scientific Opinion on the Tolerable Upper Intake Level of vitamin D". EFSA Journal 10 (7): 2813. doi:10.2903/j.efsa.2012.2813.
- ↑ "Office of Dietary Supplements – Vitamin D". https://ods.od.nih.gov/factsheets/VitaminD-Consumer/.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "PHE publishes new advice on vitamin D". Public Health England. 21 July 2016. https://www.gov.uk/government/news/phe-publishes-new-advice-on-vitamin-d.
- ↑ "Vitamin D". 18 September 2012. https://www.hsph.harvard.edu/nutritionsource/vitamin-d/.
- ↑ "Federal Register May 27, 2016 Food Labeling: Revision of the Nutrition and Supplement Facts Labels. FR page 33982.". https://www.gpo.gov/fdsys/pkg/FR-2016-05-27/pdf/2016-11867.pdf.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Daily Value Reference of the Dietary Supplement Label Database (DSLD)". https://www.dsld.nlm.nih.gov/dsld/dailyvalue.jsp.
- ↑ "Industry Resources on the Changes to the Nutrition Facts Label". 21 December 2018. https://www.fda.gov/food/food-labeling-nutrition/industry-resources-changes-nutrition-facts-label.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Vitamin D food fortification on the table". Australian Broadcasting Corporation. 12 June 2012. http://www.abc.net.au/science/articles/2012/06/12/3522708.htm.
- ↑ "Australian Health Survey: Biomedical Results for Nutrients, 2011–12". 21 December 2011. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/australian-health-survey-biomedical-results-nutrients/latest-release.
- ↑ "Vitamin D (translated)" (in sv). Swedish National Food Agency. https://www.livsmedelsverket.se/livsmedel-och-innehall/naringsamne/vitaminer-och-antioxidanter/d-vitamin.
- ↑ Vitamin-D-Bedarf bei fehlender endogener Synthese Deutsche Gesellschaft für Ernährung, January 2012
- ↑ "EMAS position statement: Vitamin D and postmenopausal health". Maturitas 71 (1): 83–8. January 2012. doi:10.1016/j.maturitas.2011.11.002. PMID 22100145.
- ↑ Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes (1997). DRI, Dietary reference intakes: for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington, D.C: National Academy Press. pp. 250. doi:10.17226/5776. ISBN 978-0-309-06350-0. http://www.nap.edu/openbook.php?isbn=0309063507&page=250. Retrieved 11 April 2010.
- ↑ "Search, National Nutrient Database for Standard Reference Release 27". US Department of Agriculture, Agricultural Research Service. 2014. http://ndb.nal.usda.gov/ndb/foods.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 133.0 133.1 "Provitamins and vitamins D2and D3in Cladina spp. over a latitudinal gradient: possible correlation with UV levels". Journal of Photochemistry and Photobiology B: Biology 62 (1–2): 118–22. September 2001. doi:10.1016/S1011-1344(01)00160-9. PMID 11693362. http://lup.lub.lu.se/record/133512. Retrieved 31 October 2018.
- ↑ "Natural vitamin D content in animal products". Advances in Nutrition 4 (4): 453–62. July 2013. doi:10.3945/an.113.003780. PMID 23858093.
- ↑ 135.0 135.1 135.2 135.3 135.4 135.5 135.6 "Photobiology of vitamin D in mushrooms and its bioavailability in humans". Dermato-Endocrinology 5 (1): 165–76. January 2013. doi:10.4161/derm.23321. PMID 24494050.
- ↑ "Vitamin D in mushrooms". Nutrient Data Laboratory, US Department of Agriculture. 2009. https://www.ars.usda.gov/ARSUserFiles/80400525/Articles/AICR09_Mushroom_VitD.pdf.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Vitamin food fortification today". Food & Nutrition Research 56: 5459. 2012. doi:10.3402/fnr.v56i0.5459. PMID 22481896.
- ↑ "Vitamin D: An overview of vitamin D status and intake in Europe". Nutrition Bulletin 39 (4): 322–350. December 2014. doi:10.1111/nbu.12108. PMID 25635171.
- ↑ "Vitamin D for Milk and Milk Alternatives". Food and Drug Administration (FDA). 15 July 2016. https://www.fda.gov/food/food-additives-petitions/vitamin-d-milk-and-milk-alternatives.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Federal Register: Food Additives Permitted for Direct Addition to Food for Human Consumption; Vitamin D2". Food and Drug Administration, US Department of Health and Human Services. 18 July 2016. https://www.federalregister.gov/documents/2016/07/18/2016-16738/food-additives-permitted-for-direct-addition-to-food-for-human-consumption-vitamin-d2.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "§172.379 Vitamin D2". Electronic Code of Federal Regulations. https://www.ecfr.gov/cgi-bin/text-idx?SID=6a3d5fc7d54cdaa0e9fd783b6063449d&mc=true&node=se21.3.172_1379&rgn=div8.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "§172.380 Vitamin D3". Electronic Code of Federal Regulations. https://www.ecfr.gov/cgi-bin/text-idx?SID=6a3d5fc7d54cdaa0e9fd783b6063449d&mc=true&node=se21.3.172_1380&rgn=div8.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Alternative to dairy milk". 16 January 2020. https://osoblanco.org/non-dairy-milk-best-alternatives-of-cow-milk/.
- ↑ "Vitamin D2 vs. vitamin D3: Are they one and the same?". Nutrition Bulletin 38 (2): 243–248. 2013. doi:10.1111/nbu.12029.
- ↑ "Vitamin D: deficiency, sufficiency and toxicity". Nutrients 5 (9): 3605–16. September 2013. doi:10.3390/nu5093605. PMID 24067388.
- ↑ "Serum concentrations of 1,25-dihydroxyvitamin D2 and 1,25-dihydroxyvitamin D3 in response to vitamin D2 and vitamin D3 supplementation". The Journal of Clinical Endocrinology and Metabolism 98 (3): 973–9. March 2013. doi:10.1210/jc.2012-2114. PMID 23386645.
- ↑ "Vitamin D bioavailability: state of the art". Critical Reviews in Food Science and Nutrition 55 (9): 1193–205. 2015. doi:10.1080/10408398.2012.688897. PMID 24915331. https://www.hal.inserm.fr/inserm-01478467/file/Vitamin%20D%20bioavailability%20HAL.pdf. Retrieved 27 April 2021.
- ↑ "Stability of vitamin D in foodstuffs during cooking". Food Chemistry 148: 170–5. April 2014. doi:10.1016/j.foodchem.2013.10.043. PMID 24262542.
- ↑ "A global representation of vitamin D status in healthy populations". Archives of Osteoporosis 7 (1–2): 155–172. 29 August 2012. doi:10.1007/s11657-012-0093-0. PMID 23225293. http://minerva-access.unimelb.edu.au/bitstream/11343/220606/1/A%20global%20representation%20of%20vitamin%20D%20status%20in%20healthy%20populations.pdf. Retrieved 20 August 2019.
- ↑ "A global representation of vitamin D status in healthy populations: reply to comment by Saadi". Archives of Osteoporosis 8 (1–2): 122. 1 February 2013. doi:10.1007/s11657-013-0122-7. PMID 23371520.
- ↑ 151.0 151.1 "25(OH)D levels in ng/mL". 19 December 2016. https://www.health.harvard.edu/blog/vitamin-d-whats-right-level-2016121910893.
- ↑ "nmol converter". http://www.endmemo.com/medical/unitconvert/Vitamin__D.php.
- ↑ "Optimal Serum 25-Hydroxyvitamin D Levels for Multiple Health Outcomes". Sunlight, Vitamin D and Skin Cancer (Review). Advances in Experimental Medicine and Biology. 810. Springer. 2008. pp. 500–25. doi:10.1007/978-0-387-77574-6_5. ISBN 978-0-387-77573-9.
- ↑ 154.0 154.1 "Plausible ergogenic effects of vitamin D on athletic performance and recovery". Journal of the International Society of Sports Nutrition 12: 33. 2015. doi:10.1186/s12970-015-0093-8. PMID 26288575.
- ↑ "Genetic and environmental determinants of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels in Hispanic and African Americans". The Journal of Clinical Endocrinology and Metabolism 93 (9): 3381–8. September 2008. doi:10.1210/jc.2007-2702. PMID 18593774.
- ↑ "Circulating 25-hydroxy-vitamin D and risk of cardiovascular disease: a meta-analysis of prospective studies". Circulation: Cardiovascular Quality and Outcomes 5 (6): 819–29. November 2012. doi:10.1161/CIRCOUTCOMES.112.967604. PMID 23149428.
- ↑ 157.0 157.1 "The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know". The Journal of Clinical Endocrinology and Metabolism 96 (1): 53–8. January 2011. doi:10.1210/jc.2010-2704. PMID 21118827.
- ↑ 158.0 158.1 158.2 Vitamin D at Merck Manual of Diagnosis and Therapy Professional Edition
- ↑ 159.0 159.1 159.2 159.3 "Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety". The American Journal of Clinical Nutrition 69 (5): 842–56. May 1999. doi:10.1093/ajcn/69.5.842. PMID 10232622. http://www.ajcn.org/content/69/5/842.full.pdf. Retrieved 30 January 2011.
- ↑ Tolerable Upper Intake Limits for Vitamins And Minerals. European Food Safety Authority. December 2006. ISBN 978-92-9199-014-6. http://www.efsa.europa.eu/en/home/oldsc/upper_level_opinions_full-part33.pdf. Retrieved 27 February 2011.
- ↑ "Mutations in CYP24A1 and idiopathic infantile hypercalcemia". The New England Journal of Medicine 365 (5): 410–21. August 2011. doi:10.1056/NEJMoa1103864. PMID 21675912.
- ↑ "CYP24A1 and SLC34A1 genetic defects associated with idiopathic infantile hypercalcemia: from genotype to phenotype". Clinical Chemistry and Laboratory Medicine 57 (11): 1650–1667. October 2019. doi:10.1515/cclm-2018-1208. PMID 31188746.
- ↑ "Vitamin D-Mediated Hypercalcemia: Mechanisms, Diagnosis, and Treatment". Endocrine Reviews 37 (5): 521–547. October 2016. doi:10.1210/er.2016-1070. PMID 27588937.
- ↑ "FDA Cautions on Accurate Vitamin D Supplementation for Infants" (Press release). Food and Drug Administration (FDA). 15 June 2010. Archived from the original on 12 January 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Regulation of calcitriol biosynthesis and activity: focus on gestational vitamin D deficiency and adverse pregnancy outcomes". Nutrients 7 (1): 443–80. January 2015. doi:10.3390/nu7010443. PMID 25584965.
- ↑ 166.0 166.1 166.2 "Trends in Use of High-Dose Vitamin D Supplements Exceeding 1000 or 4000 International Units Daily, 1999–2014". JAMA 317 (23): 2448–2450. June 2017. doi:10.1001/jama.2017.4392. PMID 28632857.
- ↑ Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium (2011). Dietary Reference Intakes for Calcium and Vitamin D. The National Academies Collection: Reports funded by National Institutes of Health. Washington (DC): National Academies Press (US). http://www.ncbi.nlm.nih.gov/books/NBK56070/. Retrieved 7 July 2012.
- ↑ 168.0 168.1 Discovering Nutrition. Jones & Bartlett Publishers. 18 March 2015. ISBN 978-1-284-06465-0. https://books.google.com/books?id=6IWHCgAAQBAJ. Retrieved 9 April 2017.
- ↑ 169.0 169.1 "Evolutionary biology and pathology of vitamin D". J Nutr Sci Vitaminol (Tokyo) Spec No: 79–83. 1992. doi:10.3177/jnsv.38.special_79. PMID 1297827.
- ↑ "Photosynthesis of vitamin D in the skin: effect of environmental and life-style variables". Federation Proceedings 46 (5): 1876–82. April 1987. PMID 3030826.
- ↑ "History of the discovery of vitamin D and its active metabolites". BoneKEy Reports 3: 479. January 2014. doi:10.1038/bonekey.2013.213. PMID 24466410.
- ↑ 172.0 172.1 "Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis". The American Journal of Clinical Nutrition 79 (3): 362–71. March 2004. doi:10.1093/ajcn/79.3.362. PMID 14985208.
- ↑ "Photolytic production of vitamin D. The preparative value of a photo-sensitiser". Journal of the Chemical Society, Chemical Communications (20): 858a. 1975. doi:10.1039/C3975000858A.
- ↑ "Serum concentrations of lipids, vitamin d metabolites, retinol, retinyl esters, tocopherols and selected carotenoids in twelve captive wild felid species at four zoos". The Journal of Nutrition 133 (1): 160–6. January 2003. doi:10.1093/jn/133.1.160. PMID 12514284.
- ↑ "Chapter 4: Photobiology of Vitamin D". Vitamin D: Volume 1: Biochemistry, Physiology and Diagnostics (4th ed.). London, UK: Academic Press. 2018. ISBN 978-0-12-809965-0.
- ↑ "Sunlight, UV Radiation, Vitamin D, and Skin Cancer: How Much Sunlight do We Need?". Sunlight, Vitamin D and Skin Cancer. Advances in Experimental Medicine and Biology. 1268. Springer. 2020. pp. 19–36. doi:10.1007/978-3-030-46227-7_2. ISBN 978-3-030-46226-0. "108 references"
- ↑ "A revised action spectrum for vitamin D synthesis by suberythemal UV radiation exposure in humans in vivo". Proceedings of the National Academy of Sciences of the United States of America 118 (40). October 2021. doi:10.1073/pnas.2015867118. PMID 34580202. Bibcode: 2021PNAS..11815867Y.
- ↑ "Vitamin D: the underappreciated D-lightful hormone that is important for skeletal and cellular health". Current Opinion in Endocrinology, Diabetes and Obesity 9 (1): 87–98. February 2002. doi:10.1097/00060793-200202000-00011.
- ↑ "Vitamin D and the skin". Journal of Bone and Mineral Metabolism 28 (2): 117–30. March 2010. doi:10.1007/s00774-009-0153-8. PMID 20107849.
- ↑ "Vitamin D: calcium and bone homeostasis during evolution". BoneKEy Reports 3: 480. January 2014. doi:10.1038/bonekey.2013.214. PMID 24466411.
- ↑ The Vitamin D Solution: A 3-Step Strategy to Cure Our Most Common Health Problems. Penguin Publishing Group. 1 April 2010. ISBN 978-1-101-22293-5. https://books.google.com/books?id=P4xbcP19H0AC. Retrieved 19 March 2023.
- ↑ Bone Loss and Osteoporosis: An Anthropological Perspective. Springer Science & Business Media. 28 June 2011. ISBN 978-1-4419-8891-1. https://books.google.com/books?id=_JV3BQAAQBAJ. "The high 25(OH)D concentrations, and relatively high vitamin D requirements of apes and monkeys are understandable in light of their biology—their body surface area relative to mass is generally greater than for humans, and they are inveterate groomers, consuming by mouth the vitamin D generated from the oils secreted by skin into fur. Although much of the vitamin D produced within human skin is absorbed directly, birds and furbearing animals acquire most of their vitamin D orally, as they groom themselves (Bicknell and Prescott, 1946; Carpenter and Zhao, 1999). Vitamin D is generated from the oily secretions of skin into fur. The oral consumption of UV-exposed dermal excretion is the way many animals acquire the "nutrient," vitamin D. Although Fraser (1983) has argued that dermal absorption of vitamin D may be more natural, what we know from animals indicates that oral consumption is equally physiological. Since vitamin D can be extracted from UV-exposed human sweat and skin secretions (Bicknell and Prescott, 1946), it is also reasonable to think that early humans obtained some of their vitamin D by mouth as well, by licking the skin."
- ↑ "Cholecalciferol supplementation alters gut function and improves digestibility in an underground inhabitant, the naked mole rat (Heterocephalus glaber), when fed on a carrot diet". The British Journal of Nutrition 69 (1): 233–41. January 1993. doi:10.1079/BJN19930025. PMID 8384476.
- ↑ "Vitamin D metabolism in dogs and cats and its relation to diseases not associated with bone metabolism". Journal of Animal Physiology and Animal Nutrition 104 (1): 322–42. January 2020. doi:10.1111/jpn.13259. PMID 31803981.
- ↑ 185.0 185.1 "The vitamin D epidemic and its health consequences". The Journal of Nutrition 135 (11): 2739S–48S. November 2005. doi:10.1093/jn/135.11.2739S. PMID 16251641. http://jn.nutrition.org/content/135/11/2739S.full.pdf. Retrieved 24 November 2011. "[Vitamin D3] is produced commercially by extracting 7-dehydrocholesterol from wool fat, followed by UVB irradiation and purification [...] [Vitamin D2] is commercially made by irradiating and then purifying the ergosterol extracted from yeast".
- ↑ "Tissue distribution of 7-dehydrocholesterol, vitamin D3 and 25-hydroxyvitamin D3 in several species of fishes". Journal of Nutritional Science and Vitaminology 32 (1): 13–22. February 1986. doi:10.3177/jnsv.32.13. PMID 3012050. https://www.jstage.jst.go.jp/article/jnsv1973/32/1/32_1_13/_pdf. Retrieved 20 August 2019.
- ↑ Göring, Horst (November 2018). "Vitamin D in Nature: A Product of Synthesis and/or Degradation of Cell Membrane Components". Biokhimiya (Moscow) 83 (11): 1350–1357. doi:10.1134/S0006297918110056. PMID 30482146. https://www.researchgate.net/publication/328961025. Retrieved 2 December 2023.
- ↑ Jäpelt, Rie B; Jakobsen, Jette (May 2013). "Vitamin D in plants: a review of occurrence, analysis, and biosynthesis". Frontiers in Plant Science 4: 136. doi:10.3389/fpls.2013.00136. PMID 23717318.
- ↑ 189.0 189.1 189.2 "Update in vitamin D". The Journal of Clinical Endocrinology and Metabolism 95 (2): 471–8. February 2010. doi:10.1210/jc.2009-1773. PMID 20133466.
- ↑ "Genetic evidence that the human CYP2R1 enzyme is a key vitamin D 25-hydroxylase". Proceedings of the National Academy of Sciences of the United States of America 101 (20): 7711–5. May 2004. doi:10.1073/pnas.0402490101. PMID 15128933. Bibcode: 2004PNAS..101.7711C.
- ↑ "Section I: Ch. 8: Vitamin D Binding Protein". Vitamin D. 1 (2 ed.). Academic Press. 2004. pp. 117–134. ISBN 978-0122526879. https://books.google.com/books?id=5c66r0KrPUMC. Retrieved 9 April 2017.
- ↑ "1,24,25-Trihydroxyvitamin D3. A metabolite of vitamin D3 effective on intestine". The Journal of Biological Chemistry 248 (19): 6691–6. October 1973. doi:10.1016/S0021-9258(19)43408-X. PMID 4355503.
- ↑ "24-Hydroxylation of 1,25-dihydroxyergocalciferol. An unambiguous deactivation process". The Journal of Biological Chemistry 261 (20): 9250–6. July 1986. doi:10.1016/S0021-9258(18)67647-1. PMID 3013880.
- ↑ "Membrane-mediated actions of 1,25-dihydroxy vitamin D3: a review of the roles of phospholipase A2 activating protein and Ca(2+)/calmodulin-dependent protein kinase II". The Journal of Steroid Biochemistry and Molecular Biology 147: 81–84. March 2015. doi:10.1016/j.jsbmb.2014.11.002. PMID 25448737.
- ↑ "The Non-Genomic Actions of Vitamin D". Nutrients 8 (3): 135. March 2016. doi:10.3390/nu8030135. PMID 26950144.
- ↑ "100 YEARS OF VITAMIN D: Historical aspects of vitamin D". Endocrine Connections 11 (4). April 2022. doi:10.1530/EC-21-0594. PMID 35245207.
- ↑ "Age-old children's disease back in force". Toronto Star. 25 July 2007. https://www.thestar.com/printarticle/239341.
- ↑ "Vitamin A, Vitamin D, Cartilage, Bones, and Teeth". Vitamins and Hormones. 21. Academic Press. 28 January 1964. pp. 51–52. ISBN 978-0-12-709821-0. https://books.google.com/books?id=gGb7vm2SapcC. Retrieved 19 March 2023.
- ↑ "History of Vitamin D". University of California at Riverside. 2011. http://vitamind.ucr.edu/about/.
- ↑ "Adolf Windaus – Biography". Nobelprize.org. 25 March 2010. http://nobelprize.org/nobel_prizes/chemistry/laureates/1928/windaus-bio.html.
- ↑ "The Ring-system of sterols and bile acids. Part II". J. Chem. Technol. Biotechnol. 51 (47): 954–7. 1932. doi:10.1002/jctb.5000514702.
- ↑ "Crystalline Vitamin D". Proceedings of the Royal Society of London. Series B, Containing Papers of a Biological Character 109 (764): 488–506. 1932. doi:10.1098/rspb.1932.0008.
- ↑ "Industrial aspects of vitamin D". Vitamin D. Academic Press. 2011. pp. 73. ISBN 978-0-12-387035-3. https://books.google.com/books?id=w7hMAFmsM84C. Retrieved 19 March 2023.
- ↑ Ivory tower and industrial innovation: university-industry technology transfer before and after the Bayh-Dole Act in the United States. Stanford Business Books. 2004. pp. 39–40. ISBN 978-0-8047-4920-6. https://books.google.com/books?id=sCscGlm2Q8YC. Retrieved 19 March 2023.
- ↑ Elbridge a Stuart: Founder of Carnation Company. Kessinger Publishing. September 2010. ISBN 978-1-164-49678-6. https://books.google.com/books?id=6fICTwEACAAJ. Retrieved 9 April 2017.
- ↑ "Chromosomal receptor for a vitamin D metabolite". Proceedings of the National Academy of Sciences of the United States of America 62 (1): 155–62. January 1969. doi:10.1073/pnas.62.1.155. PMID 5253652. Bibcode: 1969PNAS...62..155H.
- ↑ "Isolation and identification of 25-hydroxycholecalciferol from human plasma". Archives of Internal Medicine 129 (1): 56–61. January 1972. doi:10.1001/archinte.1972.00320010060005. PMID 4332591.
- ↑ "Photosynthesis of previtamin D3 in human skin and the physiologic consequences". Science 210 (4466): 203–5. October 1980. doi:10.1126/science.6251551. PMID 6251551. Bibcode: 1980Sci...210..203H.
- ↑ "Vitamin D supplementation: upper limit for safety revisited?". Aging Clin Exp Res 33 (1): 19–24. January 2021. doi:10.1007/s40520-020-01678-x. PMID 32857334.
- ↑ "ODS Vitamin D Initiative". Office of Dietary Supplements, US National Institutes of Health. 2018. https://ods.od.nih.gov/Research/VitaminD.aspx. Retrieved 22 February 2023.
- ↑ "Metabolic and immunological consequences of vitamin D deficiency in obese children". Body Metabolism and Exercise. Advances in Experimental Medicine and Biology. 840. Springer. 2015. pp. 13–9. doi:10.1007/5584_2014_81. ISBN 978-3-319-10249-8.
- ↑ "Vitamin D and cancer prevention". National Cancer Institute, US National Institutes of Health. 21 October 2013. https://www.cancer.gov/about-cancer/causes-prevention/risk/diet/vitamin-d-fact-sheet#q4.
- ↑ Goulão, Beatriz; Stewart, Fiona; Ford, John A.; MacLennan, Graeme; Avenell, Alison (2018). "Cancer and vitamin D supplementation: a systematic review and meta-analysis". The American Journal of Clinical Nutrition 107 (4): 652–63. doi:10.1093/ajcn/nqx047. PMID 29635490.
- ↑ "Effects of Nutritional Supplements and Dietary Interventions on Cardiovascular Outcomes: An Umbrella Review and Evidence Map". Annals of Internal Medicine 171 (3): 190–98. August 2019. doi:10.7326/m19-0341. PMID 31284304.
- ↑ 215.0 215.1 "Vitamin D". Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health (NIH). 26 September 2022. https://www.covid19treatmentguidelines.nih.gov/supplements/vitamin-d/.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 216.0 216.1 Template:Cite tech report
- ↑ (PDF) Evidence reviews for the use of vitamin D supplementation as prevention and treatment of COVID-19 (Report). National Institute for Health and Care Excellence (NICE). December 2020. https://www.nice.org.uk/guidance/ng187/evidence/evidence-reviews-for-the-use-of-vitamin-d-supplementation-as-prevention-and-treatment-of-covid19-pdf-8957587789. Retrieved 22 February 2021.
- ↑ "Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta-analysis". International Journal of Infectious Diseases 104: 58–64. March 2021. doi:10.1016/j.ijid.2020.12.077. PMID 33401034.
- ↑ 219.0 219.1 "Association of Vitamin D Status with SARS-CoV-2 Infection or COVID-19 Severity: A Systematic Review and Meta-analysis". Advances in Nutrition 12 (5): 1636–58. October 2021. doi:10.1093/advances/nmab012. PMID 33751020.
- ↑ 220.0 220.1 "Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies". The Journal of Steroid Biochemistry and Molecular Biology 211: 105883. July 2021. doi:10.1016/j.jsbmb.2021.105883. PMID 33775818.
- ↑ 221.0 221.1 221.2 221.3 "The link between COVID-19 and VItamin D (VIVID): A systematic review and meta-analysis". Metabolism 119: 154753. June 2021. doi:10.1016/j.metabol.2021.154753. PMID 33774074.
- ↑ 222.0 222.1 "Addendum to vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis". Critical Reviews in Food Science and Nutrition 63 (4): 557–62. August 2021. doi:10.1080/10408398.2021.1951652. PMID 34384300.
- ↑ 223.0 223.1 "Prognostic and Therapeutic Role of Vitamin D in COVID-19: Systematic Review and Meta-analysis". The Journal of Clinical Endocrinology and Metabolism 107 (5): 1484–502. April 2022. doi:10.1210/clinem/dgab892. PMID 34894254.
- ↑ "Vitamin D supplementation, COVID-19 & Disease Severity: A meta-analysis". QJM: Monthly Journal of the Association of Physicians 114 (3): 175–81. January 2021. doi:10.1093/qjmed/hcab009. PMID 33486522.
- ↑ 225.0 225.1 "Vitamin D supplementation for the treatment of COVID-19: a living systematic review". The Cochrane Database of Systematic Reviews 2021 (5): CD015043. May 2021. doi:10.1002/14651858.CD015043. PMID 34029377.
External links
 |







