Chemistry:Testosterone (medication)
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /tɛˈstɒstəroʊn/ teh-STOS-tə-rohn[1] |
| Trade names | AndroGel, Testim, TestoGel, others |
| Other names | Androst-4-en-17β-ol-3-one |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a619028 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, buccal, sublingual, intranasal, transdermal (gel, cream, patch, solution), vaginal (cream, gel, suppository), rectal (suppository), intramuscular or subcutaneous injection (oil solution, aqueous suspension), subcutaneous implant (pellet) |
| Drug class | Androgen, anabolic steroid |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Oral: very low (due to extensive first pass metabolism) |
| Metabolism | Liver (mainly reduction and conjugation) |
| Elimination half-life | 2–4 hours[citation needed] |
| Excretion | Urine (90%), feces (6%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C19H28O2 |
| Molar mass | 288.431 g·mol−1 |
| 3D model (JSmol) | |
| Specific rotation | +110.2° |
| Melting point | 155 °C (311 °F) |
| |
| |
| (verify) | |
Testosterone (T) is a medication and naturally occurring steroid hormone.[5] It is used to treat male hypogonadism, gender dysphoria, and certain types of breast cancer.[5][6] It may also be used to increase athletic ability in the form of doping.[5] It is unclear if the use of testosterone for low levels due to aging is beneficial or harmful.[7] Testosterone can be used as a gel or patch that is applied to the skin, injection into a muscle, tablet that is placed in the cheek, or tablet that is taken by mouth.[5]
Common side effects of testosterone include acne, swelling, and breast enlargement in men.[5] Serious side effects may include liver toxicity, heart disease, and behavioral changes.[5] Women and children who are exposed may develop masculinization.[5] It is recommended that individuals with prostate cancer should not use the medication.[5] It can cause harm to the baby if used during pregnancy or breastfeeding.[5] Testosterone is in the androgen family of medications.[5]
Testosterone was first isolated in 1935, and approved for medical use in 1939.[8][9] Rates of use have increased three times in the United States between 2001 and 2011.[10] It is on the World Health Organization's List of Essential Medicines.[11] It is available as a generic medication.[5] In 2020, it was the 172nd most commonly prescribed medication in the United States, with more than 3 million prescriptions.[12][13]
Medical uses
The primary use of testosterone is the treatment of males with too little or no natural testosterone production, also termed male hypogonadism or hypoandrogenism (androgen deficiency).[14] This treatment is referred to as hormone replacement therapy (HRT), or alternatively, and more specifically, as testosterone replacement therapy (TRT) or androgen replacement therapy (ART). It is used to maintain serum testosterone levels in the normal male range. Decline of testosterone production with age has led to interest in testosterone supplementation.[15]
A 2020 guideline from the American College of Physicians supports the discussion of testosterone in adult men with age-related low levels of testosterone who have sexual dysfunction. They recommend yearly evaluation regarding possible improvement and, if none, to discontinue testosterone; physicians should consider intramuscular treatments, rather than transdermal treatments, due to costs and since the effectiveness and harm of either method is similar. Testosterone treatment for reasons other than possible improvement of sexual dysfunction may not be recommended.[16][17]
Deficiency
Testosterone deficiency (also termed hypotestosteronism or hypotestosteronemia) is an abnormally low testosterone production. It may occur because of testicular dysfunction (primary hypogonadism) or hypothalamic–pituitary dysfunction (secondary hypogonadism) and may be congenital or acquired.[18]
Low levels due to aging
Testosterone levels may decline gradually with age.[19][20] The United States Food and Drug Administration (FDA) stated in 2015 that neither the benefits nor the safety of testosterone supplement have been established for low testosterone levels due to aging.[7] The FDA has required that labels on testosterone include warnings about increased risk of heart attacks and stroke.[7]
Transgender men
To take advantage of its virilizing effects, testosterone is administered to transgender men and other transmasculine individuals as part of masculinizing hormone therapy,[21] titrated to clinical effect with a "target level" of the average male's testosterone level.[22]
Women
Testosterone therapy is effective in the short-term for the treatment of hypoactive sexual desire disorder (HSDD) in women.[23] However, its long-term safety is unclear.[23] Because of a lack data to support its efficacy and safety, the Endocrine Society recommends against the routine use of testosterone in women to treat low androgen levels due to hypopituitarism, adrenal insufficiency, surgical removal of the ovaries, high-dose corticosteroid therapy, or other causes.[23] Similarly, because of a lack of data to support its efficacy and safety, the Endocrine Society recommends against the use of testosterone in women to improve general well-being, to treat infertility, sexual dysfunction due to causes other than HSDD, or to improve cognitive, cardiovascular, metabolic, and/or bone health.[23]
A 2014 systematic review and meta-analysis of 35 studies consisting of over 5,000 postmenopausal women with normal adrenal gland function found that testosterone therapy was associated with significant improvement in a variety of domains of sexual function.[24] These domains included frequency of sexual activity, orgasm, arousal, and sexual satisfaction, among others.[24] Women who were menopausal due to ovariectomy showed significantly greater improvement in sexual function with testosterone relative to those who had normal menopause.[24] In addition to beneficial effects on sexual function, testosterone was associated with unfavorable changes in blood lipids.[24] These included decreased levels of total cholesterol, triglycerides, and high-density lipoprotein (HDL) cholesterol, and increased levels of low-density lipoprotein (LDL) cholesterol.[24] However, the changes were small in magnitude, and the long-term significance in relation to cardiovascular outcomes is uncertain.[24] The changes were more pronounced with oral testosterone undecanoate than with parenteral routes, such as transdermal testosterone.[24] Testosterone showed no significant effect on depressed mood anxiety, bone mineral density (BMD), or anthropomorphic measures like body weight or body mass index.[24] Conversely, it was associated with a significant incidence of androgenic side effects, including acne and hirsutism (excessive facial/body hair growth).[24] Other androgenic side effects, such as weight gain, pattern hair loss, and voice deepening, were also reported in some trials, but were excluded from analyses due to insufficient data.[24] The overall quality of the evidence was rated as low and was considered to be inconclusive in certain areas, for instance on long-term safety.[24]
A subsequent 2017 systematic review and meta-analysis of studies including over 3,000 postmenopausal women with HSDD similarly found that short-term transdermal testosterone therapy was effective in improving multiple domains of sexual function.[25] Androgenic adverse effects such as acne and hirsutism were significantly greater in incidence with testosterone therapy, whereas no significant differences in "increase in facial hair, alopecia, voice deepening, urinary symptoms, breast pain, headache, site reaction to the patch, total adverse events, serious adverse events, reasons for withdrawal from the study, and the number of women who completed the study" were seen relative to controls.[25]
Although testosterone has been found to be effective at improving sexual function in postmenopausal women, the doses employed have been supraphysiological.[26][27] In contrast to these high doses, there is little support for the notion that testosterone is a critical hormone for sexual desire and function in women under normal physiological circumstances.[26][27] Low doses of testosterone resulting in physiological levels of testosterone (<50 ng/dL) have not been found to significantly increase sexual desire or function in women in most studies.[26] Similarly, there appears to be little or no relationship between total or free testosterone levels in the normal physiological range and sexual desire in premenopausal women.[27][26] Only high doses of testosterone resulting in supraphysiological levels of testosterone (>50 ng/dL) significantly increase sexual desire in women, with levels of testosterone of 80 to 150 ng/dL "slightly" increasing sex drive.[26][27] In accordance, men experience sexual dysfunction at testosterone levels of below 300 ng/dL, and men that have levels of testosterone of approximately 200 ng/dL frequently experience such problems.[27] The high doses of testosterone required to increase sexual desire in women may have a significant risk of masculinization with long-term therapy.[27][26] For this reason, and due to the unknown health effects and safety of testosterone therapy, its use may be inappropriate.[27][26] In 2003, the FDA rejected Intrinsa, a 300 µg/day testosterone patch for the treatment of sexual dysfunction in postmenopausal women.[26][27] The reasons cited were limited efficacy (about one additional sexually satisfying event per month), concerns about safety and potential adverse effects with long-term therapy, and concerns about inappropriate off-label use.[26][27] It appears that in women, rather than testosterone, estradiol may be the most important hormone involved in sexual desire, although data on the clinical use of estradiol to increase sexual desire in women is limited.[26][28][29]
There are no testosterone products approved for use in women in the United States and many other countries.[30] There are approved testosterone products for women in Australia (where it is considered a drug of dependence, medicines that are subject to misuse and trafficking.[31]) and some European countries.[30] Testosterone pellet implants are approved for use in postmenopausal women in the United Kingdom.[32][33] Testosterone products for men can be used off-label in women in the United States.[30] Alternatively, testosterone products for women are available from compounding pharmacies in the United States, although such products are unregulated and manufacturing quality is not ensured.[34]
| Route | Medication | Form | Dosage | |
|---|---|---|---|---|
| Oral | Methyltestosterone | Tablet | 30–200 mg/day | |
| Fluoxymesterone | Tablet | 10–40 mg 3x/day | ||
| Calusterone | Tablet | 40–80 mg 4x/day | ||
| Normethandrone | Tablet | 40 mg/day | ||
| Buccal | Methyltestosterone | Tablet | 25–100 mg/day | |
| Injection (IM or SC) | Testosterone propionate | Oil solution | 50–100 mg 3x/week | |
| Testosterone enanthate | Oil solution | 200–400 mg 1x/2–4 weeks | ||
| Testosterone cypionate | Oil solution | 200–400 mg 1x/2–4 weeks | ||
| Mixed testosterone esters | Oil solution | 250 mg 1x/week | ||
| Methandriol | Aqueous suspension | 100 mg 3x/week | ||
| Androstanolone (DHT) | Aqueous suspension | 300 mg 3x/week | ||
| Drostanolone propionate | Oil solution | 100 mg 1–3x/week | ||
| Metenolone enanthate | Oil solution | 400 mg 3x/week | ||
| Nandrolone decanoate | Oil solution | 50–100 mg 1x/1–3 weeks | ||
| Nandrolone phenylpropionate | Oil solution | 50–100 mg/week | ||
| Note: Dosages are not necessarily equivalent. Sources: See template. | ||||
Available forms
Testosterone has been marketed for use by oral, sublingual, buccal, intranasal, transdermal (patches), topical (gels), intramuscular (injection), and subcutaneous (implant) administration.[35][36][37][38] It is provided unmodified and as a testosterone ester such as testosterone cypionate, testosterone enanthate, testosterone propionate, or testosterone undecanoate, which act as prodrugs of testosterone.[35][36][37] The most common route of administration for testosterone is by intramuscular injection.[35] However, it has been reported that AndroGel, a transdermal gel formulation of testosterone, has become the most popular form of testosterone in androgen replacement therapy for hypogonadism in the United States.[36]
Non-medical use
Athletics
Testosterone is used as a form of doping among athletes in order to improve performance.[39] Testosterone is classified as an anabolic agent and is on the World Anti-Doping Agency (WADA) List of Prohibited Substances and Methods.[39] Hormone supplements cause the endocrine system to adjust its production and lower the natural production of the hormone, so when supplements are discontinued, natural hormone production is lower than it was originally.[citation needed]
Anabolic–androgenic steroids (AAS), including testosterone and its esters, have also been taken to enhance muscle development, strength, or endurance. They do so directly by increasing the muscles' protein synthesis. As a result, muscle fibers become larger and repair faster than the average person's.[citation needed]
After a series of scandals and publicity in the 1980s (such as Ben Johnson's improved performance at the 1988 Summer Olympics), prohibitions of AAS use were renewed or strengthened by many sports organizations. Testosterone and other AAS were designated a "controlled substance" by the United States Congress in 1990, with the Anabolic Steroid Control Act.[40] Their use is seen as an issue in modern sport, particularly given the lengths to which athletes and professional laboratories go to in trying to conceal such use from sports regulators. Steroid use once again came into the spotlight as a result of Canadian professional wrestler Chris Benoit's double murder-suicide in 2007; however, there is no evidence implicating steroid use as a factor in the incident.[citation needed]
Some female athletes may have naturally higher levels of testosterone than others, and may be asked to consent to sex verification and either surgery or drugs to decrease testosterone levels.[41] This has proven contentious, with the Court of Arbitration for Sport suspending the IAAF policy due to insufficient evidence of a link between high androgen levels and improved athletic performance.[42][43]
Detection of abuse
A number of methods for detecting testosterone use by athletes have been employed, most based on a urine test. These include the testosterone/epitestosterone ratio (normally less than 6), the testosterone/luteinizing hormone ratio and the carbon-13/carbon-12 ratio (pharmaceutical testosterone contains less carbon-13 than endogenous testosterone). In some testing programs, an individual's own historical results may serve as a reference interval for interpretation of a suspicious finding. Another approach being investigated is the detection of the administered form of testosterone, usually an ester, in hair.[44][45][46][47]
Contraindications
Absolute contraindications of testosterone include prostate cancer, elevated hematocrit (>54%), uncontrolled congestive heart failure, various other cardiovascular diseases, and uncontrolled obstructive sleep apnea.[48] Breast cancer is said by some sources to be an absolute contraindication of testosterone therapy,[48] but androgens including testosterone have also actually been used to treat breast cancer.[49] Relative contraindications of testosterone include elevated prostate-specific antigen (PSA) in men with a high risk of prostate cancer due to ethnicity or family history, severe lower urinary tract symptoms, and elevated hematocrit (>50%).[48]
Side effects
Adverse effects may also include minor side effects such as oily skin, acne, and seborrhea, as well as loss of scalp hair, which may be prevented or reduced with 5α-reductase inhibitors. In women, testosterone can produce hirsutism (excessive facial/body hair growth), deepening of the voice, and other signs of virilization. Exogenous testosterone may cause suppression of spermatogenesis in men, leading to, in some cases, reversible infertility.[50] Gynecomastia and breast tenderness may occur with high dosages of testosterone due to peripheral conversion of testosterone by aromatase into excessive amounts of the estrogen estradiol.[51] Testosterone treatment, particularly in high dosages, can also be associated with mood changes, increased aggression, increased sex drive, spontaneous erections, and nocturnal emissions.[52][53][54][55]
Other side effects include increased hematocrit, which can require venipuncture in order to treat, and exacerbation of sleep apnea.[56]
The FDA stated in 2015 that neither the benefits nor the safety of testosterone have been established for low testosterone levels due to aging.[7] The FDA has required that testosterone pharmaceutical labels include warning information about the possibility of an increased risk of heart attacks and stroke.[7] They have also required the label include concerns about abuse and dependence.[57]
Injectable forms of testosterone can cause a lung problem called pulmonary oil microembolism (POME). Symptoms of POME include cough, shortness of breath, tightening of the throat, chest pain, sweating, dizziness, and fainting.[58][59] A postmarketing analysis by the manufacturer of Aveed (testosterone undeconate injection) found that POME occurred at a rate of less than 1% per injection per year for Aveed.[60]
Long-term adverse effects
Cardiovascular disease
Adverse effects of testosterone supplementation may include increased cardiovascular events (including strokes and heart attacks) and deaths based on three peer-reviewed studies involving men taking testosterone replacement.[61] In addition, an increase of 30% in deaths and heart attacks in older men has been reported.[62] Due to an increased incidence of adverse cardiovascular events compared to a placebo group, a Testosterone in Older Men with Mobility Limitations (TOM) trial (a National Institute of Aging randomized trial) was halted early by the Data Safety and Monitoring Committee.[63] On January 31, 2014, reports of strokes, heart attacks, and deaths in men taking FDA-approved testosterone-replacement led the FDA to announce that it would be investigating the issue.[64] Later, in September 2014, the FDA announced, as a result of the "potential for adverse cardiovascular outcomes", a review of the appropriateness and safety of Testosterone Replacement Therapy (TRT).[65][66][67] The FDA now requires warnings in the drug labeling of all approved testosterone products regarding deep vein thrombosis and pulmonary embolism.[68]
Up to the year 2010, studies had not shown any effect on the risk of death, prostate cancer or cardiovascular disease;[69][70] more recent[when?] studies, however, do raise concerns.[71] A 2013 study, published in the Journal of the American Medical Association, reported "the use of testosterone therapy was significantly associated with increased risk of adverse outcomes." The study began after a previous, randomized, clinical trial of testosterone therapy in men was stopped prematurely "due to adverse cardiovascular events raising concerns about testosterone therapy safety."[62]
However, when given to men with hypogonadism in the short- and medium-term, testosterone replacement therapy does not increase the risk of cardiovascular events (including strokes and heart attacks and other heart diseases). The long-term safety of the therapy is not known yet.[72][73]
Prostate cancer
Testosterone in the presence of a slow-growing prostate cancer is assumed to increase its growth rate. However, the association between testosterone supplementation and the development of prostate cancer is unproven.[74] Nevertheless, physicians are cautioned about the cancer risk associated with testosterone supplementation.[75]
Testosterone may accelerate pre-existing prostate cancer growth in individuals who have undergone androgen deprivation.[56] It is recommended that physicians screen for prostate cancer with a digital rectal exam and prostate-specific antigen (PSA) level before starting therapy, and monitor PSA and hematocrit levels closely during therapy.[19]
Ethnic groups have different rates of prostate cancer.[76] Differences in sex hormones, including testosterone, have been suggested as an explanation for these differences.[76] This apparent paradox can be resolved by noting that prostate cancer is very common. In autopsies, 80% of 80-year-old men have prostate cancer.[77]
Pregnancy and breastfeeding
Testosterone is contraindicated in pregnancy and not recommended during breastfeeding.[78] Androgens like testosterone are teratogens and are known to cause fetal harm, such as producing virilization and ambiguous genitalia.
Interactions
5α-Reductase inhibitors
5α-Reductase inhibitors like finasteride and dutasteride can slightly increase circulating levels of testosterone by inhibiting its metabolism.[79] However, these drugs do this via prevention of the conversion of testosterone into its more potent metabolite dihydrotestosterone (DHT), and this results in dramatically reduced circulating levels of DHT (which circulates at much lower relative concentrations).[79][80] In addition, local levels of DHT in so-called androgenic (5α-reductase-expressing) tissues are also markedly reduced,[79][80] and this can have a strong impact on certain effects of testosterone.[37][81] For instance, growth of body and facial hair and penile growth induced by testosterone may be inhibited by 5α-reductase inhibitors, and this could be considered undesirable in the context of, for instance, puberty induction.[81][82] On the other hand, 5α-reductase inhibitors may prevent or reduce adverse androgenic side effects of testosterone like scalp hair loss, oily skin, acne, and seborrhea.[37] In addition to the prevention of testosterone conversion into DHT, 5α-reductase inhibitors also prevent the formation of neurosteroids like 3α-androstanediol from testosterone, and this may have neuropsychiatric consequences in some men.[83]
Aromatase inhibitors
Aromatase inhibitors like anastrozole prevent the conversion of testosterone into estradiol by aromatase.[37] As only a very small fraction of testosterone is converted into estradiol, this does not affect testosterone levels, but it can prevent estrogenic side effects like gynecomastia that can occur when testosterone is administered at relatively high dosages.[37] However, estradiol exerts negative feedback on the hypothalamic–pituitary–gonadal axis and, for this reason, prevention of its formation can reduce this feedback and disinhibit gonadal production of testosterone, which in turn can increase levels of endogenous testosterone.[84] Testosterone therapy is sometimes combined with an aromatase inhibitor for men with secondary hypogonadism who wish to conceive children with their partners.[85]
Cytochrome P450 inhibitors
Inhibitors and inducers of cytochrome P450 enzymes like CYP3A4 have been associated with little or no effect on circulating testosterone levels.[citation needed]
Antiandrogens and estrogens
Antiandrogens like cyproterone acetate, spironolactone, and bicalutamide can block the androgenic and anabolic effects of testosterone.[86][87] Estrogens can reduce the effects of testosterone by increasing the hepatic production and in turn circulating levels of sex hormone-binding globulin (SHBG), a carrier protein that binds to and occupies androgens like testosterone and DHT, and thereby reducing free concentrations of these androgens.[87][88]
Pharmacology
Pharmacodynamics
| Medication | Ratioa |
|---|---|
| Testosterone | ~1:1 |
| Androstanolone (DHT) | ~1:1 |
| Methyltestosterone | ~1:1 |
| Methandriol | ~1:1 |
| Fluoxymesterone | 1:1–1:15 |
| Metandienone | 1:1–1:8 |
| Drostanolone | 1:3–1:4 |
| Metenolone | 1:2–1:30 |
| Oxymetholone | 1:2–1:9 |
| Oxandrolone | 1:3–1:13 |
| Stanozolol | 1:1–1:30 |
| Nandrolone | 1:3–1:16 |
| Ethylestrenol | 1:2–1:19 |
| Norethandrolone | 1:1–1:20 |
| Notes: In rodents. Footnotes: a = Ratio of androgenic to anabolic activity. Sources: See template. | |
Testosterone is a high affinity ligand for and agonist of the nuclear androgen receptor (AR). In addition, testosterone binds to and activates membrane androgen receptors (mARs) such as GPRC6A and ZIP9. Testosterone is also potentiated via transformation by 5α-reductase into the more potent androgen DHT in so-called androgenic tissues such as the prostate gland, seminal vesicles, skin, and hair follicles. In contrast to the case of testosterone, such potentiation occurs to a reduced extent or not at all with most synthetic AAS (as well as with DHT), and this is primarily responsible for the dissociation of anabolic and androgenic effects with these agents.[89] In addition to DHT, testosterone is converted at a rate of approximately 0.3% into the estrogen estradiol via aromatase.[90] This occurs in many tissues, especially adipose tissue, the liver, and the brain, but primarily in adipose tissue.[90] Testosterone, after conversion into DHT, is also metabolized into 3α-androstanediol, a neurosteroid and potent positive allosteric modulator of the GABAA receptor, and 3β-androstanediol, a potent and preferential agonist of the ERβ.[91] These metabolites, along with estradiol, may be involved in a number of the effects of testosterone in the brain, including its antidepressant, anxiolytic, stress-relieving, rewarding, and pro-sexual effects.[91]
Effects in the body and brain
The ARs are expressed widely throughout the body, including in the penis, testicles, epididymides, prostate gland, seminal vesicles, fat, skin, bone, bone marrow, muscle, larynx, heart, liver, kidneys, pituitary gland, hypothalamus, and elsewhere throughout the brain.[92][93] Through activation of the ARs (as well as the mARs), testosterone has many effects, including the following:[92][35][additional citation(s) needed]
- Promotes growth, function, and maintenance of the prostate gland, seminal vesicles, and penis during puberty and thereafter
- Promotes growth and maintenance of muscles, particularly of the upper body
- Causes subcutaneous fat to be deposited in a masculine pattern and decreases overall body fat
- Suppresses breast development induced by estrogens, but can also still produce gynecomastia via excessive conversion into estradiol if levels are too high
- Maintains skin health, integrity, appearance, and hydration and slows the rate of aging of the skin, but can also cause oily skin, acne, and seborrhea
- Promotes the growth of facial and body hair, but can also cause scalp hair loss and hirsutism
- Contributes to bone growth and causes broadening of the shoulders at puberty
- Modulates liver protein synthesis, such as the production of sex hormone-binding globulin and many other proteins
- Increases production of erythropoietin in the kidneys and thereby stimulates red blood cell production in bone marrow and elevates hematocrit
- Exerts negative feedback on the hypothalamic–pituitary–gonadal axis by suppressing the secretion of the gonadotropins follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary gland, thereby inhibiting gonadal sex hormone production as well as spermatogenesis and fertility
- Regulates the vasomotor system and body temperature via the hypothalamus, thereby preventing hot flashes
- Modulates brain function, with effects on mood, emotionality, aggression, and sexuality, as well as cognition and memory
- Increases sex drive and erectile capacity and causes spontaneous erections and nocturnal emissions
- Increases the risk of benign prostatic hyperplasia and prostate cancer and accelerates the progression of prostate cancer
- Decreases breast proliferation and the risk of breast cancer
Pharmacokinetics
Testosterone can be taken by a variety of different routes of administration.[94] These include oral, buccal, sublingual, intranasal, transdermal (gels, creams, patches), rectal suppositories), by intramuscular or subcutaneous injection (in oil or aqueous), and as a subcutaneous implant.[94] The pharmacokinetics of testosterone, including its bioavailability, circulating testosterone levels, metabolism, biological half-life, and other parameters, differ by route of administration.[94]
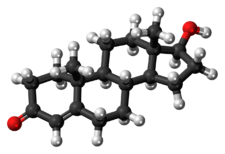
Chemistry
Testosterone is a naturally occurring androstane steroid and is also known by the chemical name androst-4-en-17β-ol-3-one.[95] It has a double bond between the C4 and C5 positions (making it an androstene), a ketone group at the C3 position, and a hydroxyl (alcohol) group at the C17β position.[95]
Derivatives
Testosterone esters are substituted at the C17β position with a lipophilic fatty acid ester moiety of varying chain length.[96] Major testosterone esters include testosterone cypionate, testosterone enanthate, testosterone propionate, and testosterone undecanoate.[87][95][97] A C17β ether prodrug of testosterone, cloxotestosterone acetate, has also been marketed, although it is little known and is used very rarely or no longer.[95] Another C17β ether prodrug of testosterone, silandrone, also exists but was never marketed, and is notable in that it is orally active.[95] In addition to ester and ether prodrugs, androgen prohormones or precursors of testosterone, such as dehydroepiandrosterone (DHEA), androstenediol, and androstenedione, exist as well, and convert into testosterone to variable extents upon oral ingestion.[98] Unlike testosterone ester and ether prodrugs however, these prohormones are only weakly androgenic/anabolic.[98]
All synthetic AAS are derivatives of testosterone.[98] Prominent examples include nandrolone (19-nortestosterone), metandienone (17α-methyl-δ1-testosterone), and stanozolol (a 17α-alkylated derivative of DHT). Unlike testosterone, AAS that are 17α-alkylated, like metandienone and stanozolol, are orally active. This is due to steric hindrance of C17β-position metabolism during the first-pass through the liver. In contrast, most AAS that are not 17α-alkylated, like nandrolone, are not active orally, and must instead be administered via intramuscular injection. This is almost always in ester form; for instance, in the case of nandrolone, as nandrolone decanoate or nandrolone phenylpropionate.
History
Testosterone was first isolated and synthesized in 1935.[99] Shortly thereafter, in 1937, testosterone first became commercially available as a pharmaceutical drug in the form of pellets and then in ester form for intramuscular injection as the relatively short-acting testosterone propionate.[37][35][100] Methyltestosterone, one of the first synthetic AAS and orally active androgens, was introduced in 1935, but was associated with hepatotoxicity and eventually became largely medically obsolete.[100] In the mid-1950s, the longer-acting testosterone esters testosterone enanthate and testosterone cypionate were introduced.[100] They largely superseded testosterone propionate and became the major testosterone esters used medically for over half a century.[100] In the 1970s, testosterone undecanoate was introduced for oral use in Europe,[100] although intramuscular testosterone undecanoate had already been in use in China for several years.[101] Intramuscular testosterone undecanoate was not introduced in Europe and the United States until much later (in the early to mid 2000s and 2014, respectively).[102][103]
The history of testosterone as a medication has been reviewed.[104][105][106][107]
Society and culture
Usage
In the US in the 2000s, companies and figures in the popular media have heavily marketed notions of "andropause" as something parallel to menopause; these notions have been rejected by the medical community.[108][109] Additionally, advertising from drug companies selling testosterone and human growth hormone, as well as dietary supplement companies selling all kinds of "boosters" for aging men, have emphasized the "need" of middle-aged or ageing men for testosterone.[110] There is a medical condition called late-onset hypogonadism; according to Thomas Perls and David J. Handelsman, writing in a 2015 editorial in the Journal of the American Geriatrics Society, it appears that this condition is overdiagnosed and overtreated.[110] Perls and Handelsman note that in the US, "sales of testosterone increased from $324 million in 2002 to $2 billion in 2012, and the number of testosterone doses prescribed climbed from 100 million in 2007 to half a billion in 2012, not including the additional contributions from compounding pharmacies, Internet, and direct-to-patient clinic sales."[110]
Generic names
Testosterone is the generic name of testosterone in English and Italian and the INN, USAN, USP, BAN, and DCIT of the drug, while testostérone is its French name and the DCF.[95][111][112] It is also referred to in Latin as testosteronum, in Spanish and Portuguese as testosterona, and in German, Dutch, and Russian and other Slavic languages as testosteron.[111][112] The Cyrillic script of testosterone is тестостерон.[113]
Brand names
Testosterone is marketed under a large number of brand names throughout the world.[111] Major brand names of testosterone and/or its esters include Andriol, Androderm, AndroGel, Axiron, Delatestryl, Depo-Testosterone, Intrinsa, Nebido, Omnadren, Primoteston, Sustanon, Testim, TestoGel, TestoPatch, Testoviron, and Tostran.[87][89][111]
Availability
United States
(As of November 2016), unmodified (non-esterified) testosterone is available in the United States in the following formulations:[114]
- Topical gels: AndroGel, Fortesta, Testim, Testosterone (generic)
- Topical solutions: Axiron, Testosterone (generic)
- Transdermal patches: Androderm, Testoderm (discontinued), Testoderm TTS (discontinued), Testosterone (generic)
- Intranasal gels: Natesto
- Buccal tablets: Striant
- Pellet implants: Testopel
And the following ester prodrugs of testosterone are available in the United States in oil solutions for intramuscular injection:[114]
- Testosterone cypionate: Depo-Testosterone, Testosterone Cypionate (generic)
- Testosterone enanthate: Delatestryl, Xyosted (auto-injector), Testosterone Enanthate (generic)
- Testosterone propionate: Testosterone Propionate (generic)
- Testosterone undecanoate: Aveed
Unmodified testosterone was also formerly available for intramuscular injection but was discontinued.[114]
Testosterone cypionate and testosterone enanthate were formerly available in combination with estradiol cypionate and estradiol valerate, respectively, under the brand names Depo-Testadiol and Ditate-DS, respectively, as oil solutions for intramuscular injection, but these formulations have been discontinued.[114]
Unlike in Europe, Canada, and much of the rest of the world, oral testosterone undecanoate is not available in the United States.[114][115][116]
Canada
(As of November 2016), testosterone is available in Canada in the form of topical gels (AndroGel, Testim), topical solutions (Axiron), transdermal patches (Androderm), and intranasal gels (Natesto).[117] Testosterone cypionate (Depo-Testosterone, Testosterone Cypionate (generic)), testosterone enanthate (Delatestryl, PMS-Testosterone Enanthate), and testosterone propionate (Testosterone Propionate (generic)) are available as oil solutions for intramuscular injection and testosterone undecanoate (Andriol, PMS-Testosterone, Taro-Testosterone) is available in the form of oral capsules.[117] Testosterone buccal tablets and pellet implants do not appear to be available in Canada.[117]
Other countries
Testosterone and/or its esters are widely available in countries throughout the world in a variety of formulations.[111]
Legal status
Testosterone and its esters, along with other AAS, are prescription-only controlled substances in many countries throughout the world. In the United States, they are Schedule III drugs under the Controlled Substances Act, in Canada, they are Schedule IV drugs under the Controlled Drugs and Substances Act, and in the United Kingdom, they are Class C drugs under the Misuse of Drugs Act.[118][119]
Litigation
Doping in sports
There are many known cases of doping in sports with testosterone and its esters by professional athletes.
Research
Depression
Testosterone has been used to treat depression in men who are of middle age with low testosterone. However, a 2014 review showed no benefit on the mood of the men with normal levels of testosterone or on the mood of the older men with low testosterone.[120] Conversely, a 2009 review found that testosterone had an antidepressant effect in men with depression, especially those with hypogonadism, HIV/AIDS, and in the elderly.[121]
Heart failure
Testosterone replacement can significantly improve exercise capacity, muscle strength and reduce QT intervals in men with chronic heart failure (CHF). Over the 3 to 6-month course of the studies reviewed, testosterone therapy appeared safe and generally effective, and (ruling out prostate cancer) the authors found no justification to absolutely restrict its use in men with CHF.[122] A similar 2012 review also found increased exercise capacity and reasoned the benefits generlizable to women.[123] However, both reviews advocate larger, longer term, randomized controlled trials.[122][123]
Male contraception
Testosterone, as esters such as testosterone undecanoate or testosterone buciclate, has been studied and promoted as a male contraceptive analogous to estrogen-based contraceptives in women. Otherwise considered an adverse effect of testosterone, reduced spermatogenesis can be further suppressed with the addition of a progestin such as norethisterone enanthate or levonorgestrel butanoate, improving the contraceptive effect.[124][125]
Anorgasmia
Testosterone is under development in a low-dose intranasal formulation for the treatment of anorgasmia in women.[126]
Miscellaneous
Testosterone therapy may improve the management of type 2 diabetes.[127] Low testosterone has been associated with the development of Alzheimer's disease.[128][129]
Topical androgens like testosterone have been used and studied in the treatment of cellulite in women.[130]
References
- ↑ Testosterone. Oxford Dictionaries.
- ↑ "Testosterone Use During Pregnancy". 20 August 2019. https://www.drugs.com/pregnancy/testosterone.html.
- ↑ Human Medicines Evaluation Division (1 September 2022). "Active substance: testosterone (all formulations apart from topical use)". List of nationally authorised medicinal products. European Medicines Agency. https://www.ema.europa.eu/documents/psusa/testosterone-all-formulations-apart-topical-use-list-nationally-authorised-medicinal-products-psusa/00010631/202112_en.pdf.
- ↑ Human Medicines Evaluation Division (1 September 2022). "Active substance: testosterone (topical use)". List of nationally authorised medicinal products. European Medicines Agency. https://www.ema.europa.eu/documents/psusa/testosterone-topical-use-list-nationally-authorised-medicinal-products-psusa/00002908/202112_en.pdf.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 "Testosterone". American Society of Health-System Pharmacists. December 4, 2015. https://www.drugs.com/monograph/testosterone.html.
- ↑ "List of Gender Dysphoria Medications (6 Compared)" (in en). https://www.drugs.com/condition/gender-dysphoria.html.
- ↑ 7.0 7.1 7.2 7.3 7.4 Staff (3 March 2015). "Testosterone Products: Drug Safety Communication – FDA Cautions About Using Testosterone Products for Low Testosterone Due to Aging; Requires Labeling Change to Inform of Possible Increased Risk of Heart Attack And Stroke". FDA. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm436280.htm.
- ↑ Anabolic Steroids and the Athlete (2nd ed.). McFarland. 2002. p. 180. ISBN 978-0-7864-1128-3. https://books.google.com/books?id=OGcQ0Tp2AFcC&pg=PA180.
- ↑ (in en) Analogue-based Drug Discovery. John Wiley & Sons. 2006. p. 481. ISBN 9783527607495. https://books.google.com/books?id=FjKfqkaKkAAC&pg=PA481. Retrieved August 18, 2020.
- ↑ "Testosterone therapy in the new era of Food and Drug Administration oversight". Translational Andrology and Urology 5 (2): 207–12. April 2016. doi:10.21037/tau.2016.03.13. PMID 27141448.
- ↑ World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. 2019. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ "The Top 300 of 2020". https://clincalc.com/DrugStats/Top300Drugs.aspx.
- ↑ "Testosterone - Drug Usage Statistics". https://clincalc.com/DrugStats/Drugs/Testosterone.
- ↑ "Testosterone treatments: why, when, and how?". American Family Physician 73 (9): 1591–8. May 2006. PMID 16719252. http://www.aafp.org/afp/2006/0501/p1591.html. Retrieved 2016-10-03.
- ↑ "Androgen replacement therapy in the aging male". Reviews in Urology 5 (4): 216–26. 2003. PMID 16985841.
- ↑ "Testosterone Treatment in Adult Men With Age-Related Low Testosterone: A Clinical Guideline From the American College of Physicians". Annals of Internal Medicine 172 (2): 126–133. January 2020. doi:10.7326/M19-0882. PMID 31905405.
- ↑ "New Guideline for Testosterone Treatment in Men With 'Low T'". Medscape.com. 7 January 2020. https://www.medscape.com/viewarticle/923449.
- ↑ "The male menopause: does it exist?: for: some men need investigation and testosterone treatment". The Western Journal of Medicine 173 (2): 76–8. Aug 2000. doi:10.1136/ewjm.173.2.76. PMID 10924412.
- ↑ 19.0 19.1 "Introduction". Testosterone and Aging: Clinical Research Directions.. National Academies Press (US). January 1, 2004. doi:10.17226/10852. ISBN 978-0-309-09063-6. https://www.ncbi.nlm.nih.gov/books/NBK216164/. Retrieved November 11, 2016.
- ↑ "In men older than 70 years, total testosterone remains stable while free testosterone declines with age. The Health in Men Study". European Journal of Endocrinology 156 (5): 585–94. May 2007. doi:10.1530/EJE-06-0714. PMID 17468195.
- ↑ "Gender dysphoria – Treatment". NHS Gov.uk. May 21, 2012. http://www.nhs.uk/Conditions/Gender-dysphoria/Pages/Treatment.aspx.
- ↑ "Medical Therapy and Health Maintenance for Transgender Men: A Guide For Health Care Providers". Lyon-Martin Women's Health Services. http://www.nickgorton.org/Medical%20Therapy%20and%20HM%20for%20Transgender%20Men_2005.pdf.
- ↑ 23.0 23.1 23.2 23.3 "Androgen therapy in women: a reappraisal: an Endocrine Society clinical practice guideline". The Journal of Clinical Endocrinology and Metabolism 99 (10): 3489–510. Oct 2014. doi:10.1210/jc.2014-2260. PMID 25279570.
- ↑ 24.00 24.01 24.02 24.03 24.04 24.05 24.06 24.07 24.08 24.09 24.10 "Clinical review: The benefits and harms of systemic testosterone therapy in postmenopausal women with normal adrenal function: a systematic review and meta-analysis". J. Clin. Endocrinol. Metab. 99 (10): 3543–50. 2014. doi:10.1210/jc.2014-2262. PMID 25279572.
- ↑ 25.0 25.1 "Efficacy and safety of transdermal testosterone in postmenopausal women with hypoactive sexual desire disorder: a systematic review and meta-analysis". Fertil. Steril. 107 (2): 475–482.e15. 2017. doi:10.1016/j.fertnstert.2016.10.028. PMID 27916205.
- ↑ 26.0 26.1 26.2 26.3 26.4 26.5 26.6 26.7 26.8 26.9 "Increasing women's sexual desire: The comparative effectiveness of estrogens and androgens". Horm Behav 78: 178–93. February 2016. doi:10.1016/j.yhbeh.2015.11.003. PMID 26589379.
- ↑ 27.0 27.1 27.2 27.3 27.4 27.5 27.6 27.7 27.8 "Has testosterone passed the test in premenopausal women with low libido? A systematic review". Int J Women's Health 8: 599–607. 2016. doi:10.2147/IJWH.S116212. PMID 27785108.
- ↑ "Role of Estrogens and Estrogen-Like Compounds in Female Sexual Function and Dysfunction". J Sex Med 13 (3): 305–16. March 2016. doi:10.1016/j.jsxm.2015.11.015. PMID 26944462.
- ↑ "Sexual medicine: Transdermal oestrogen is effective". Nat Rev Urol 14 (11): 638. November 2017. doi:10.1038/nrurol.2017.152. PMID 28895561.
- ↑ 30.0 30.1 30.2 Essentials of Menopause Management: A Case-Based Approach. Springer. 21 January 2017. pp. 180–. ISBN 978-3-319-42451-4. https://books.google.com/books?id=HVkLDgAAQBAJ&pg=PA180. Retrieved July 31, 2018.
- ↑ "Drugs of dependence and drug-dependent persons". Department of Health. Victorian Government. http://www.health.vic.gov.au/drugs-and-poisons/drugs-of-dependence-and-drug-dependent-persons.
- ↑ Menopause: Biology and Pathobiology. Academic Press. 22 May 2000. pp. 454–. ISBN 978-0-08-053620-0. https://books.google.com/books?id=i9HXKhjvNVAC&pg=PA454. Retrieved September 27, 2018.
- ↑ Androgens in Health and Disease. Springer Science & Business Media. 27 May 2003. pp. 374–. ISBN 978-1-59259-388-0. https://books.google.com/books?id=vDcBCAAAQBAJ&pg=PA374. Retrieved September 27, 2018.
- ↑ "Custom-compounded bioidentical hormone therapy: why so popular despite potential harm? The case against routine use". Climacteric 20 (3): 205–211. June 2017. doi:10.1080/13697137.2017.1285277. PMID 28509626.
- ↑ 35.0 35.1 35.2 35.3 35.4 Testosterone: Action - Deficiency - Substitution. Springer Science & Business Media. 6 December 2012. pp. 1–,9,298,309–331,349–353,366–367. ISBN 978-3-642-72185-4. https://books.google.com/books?id=jn3nCAAAQBAJ&pg=PA350. Retrieved November 18, 2016.
- ↑ 36.0 36.1 36.2 Cite error: Invalid
<ref>tag; no text was provided for refs namedMelmed2016 - ↑ 37.0 37.1 37.2 37.3 37.4 37.5 37.6 Anabolics. Molecular Nutrition Llc. 2011. pp. 385–394, 413, 426, 607, 666. ISBN 978-0-9828280-1-4. https://books.google.com/books?id=afKLA-6wW0oC&pg=PT385. Retrieved December 18, 2017.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedBrotherton1976 - ↑ 39.0 39.1 "S1. Anabolic Agents | List of Prohibited Substances and Methods". http://list.wada-ama.org/list/s1-anabolic-agents.
- ↑ "Anabolic Steroid Control Act". United States Sentencing Commission. 1990. http://www.ussc.gov/USSCsteroidsreport-0306.pdf#search=%22Anabolic%20Steroid%20Control%20Act%20of%201990%22.
- ↑ "The Trouble With Too Much T". The New York Times. April 11, 2014. https://www.nytimes.com/2014/04/11/opinion/the-trouble-with-too-much-t.html.
- ↑ "Katie Ledecky is crushing records, so why are we still worried about Caster Semenya?". ESPN. August 13, 2016. http://www.espn.com/espnw/voices/article/17275159/.
- ↑ "The Humiliating Practice of Sex-Testing Female Athletes". The New York Times. June 28, 2016. ISSN 0362-4331. https://www.nytimes.com/2016/07/03/magazine/the-humiliating-practice-of-sex-testing-female-athletes.html.
- ↑ "Detection of testosterone administration based on the carbon isotope ratio profiling of endogenous steroids: international reference populations of professional soccer players". British Journal of Sports Medicine 43 (13): 1041–44. Dec 2009. doi:10.1136/bjsm.2009.058669. PMID 19549614.
- ↑ "Subject-based profiling for the detection of testosterone administration in sport". Drug Testing and Analysis 1 (1): 22–4. Jan 2009. doi:10.1002/dta.14. PMID 20355155.
- ↑ "Quantification of testosterone undecanoate in human hair by liquid chromatography-tandem mass spectrometry". Biomedical Chromatography 23 (8): 873–80. Aug 2009. doi:10.1002/bmc.1199. PMID 19353724.
- ↑ Disposition of Toxic Drugs & Chemicals in Man (8th ed.). Foster City, Calif: Biomedical Publications. 2008. pp. 1501–04. ISBN 978-0-9626523-7-0.
- ↑ 48.0 48.1 48.2 Clinical Urologic Endocrinology: Principles for Men's Health. Springer Science & Business Media. 19 October 2012. pp. 65–. ISBN 978-1-4471-4405-2. https://books.google.com/books?id=Eko5nLSINv8C&pg=PA65. Retrieved November 13, 2016.
- ↑ The Chemotherapy Source Book. Lippincott Williams & Wilkins. 2008. pp. 368–. ISBN 978-0-7817-7328-7. https://books.google.com/books?id=CDADMzS0TKUC&pg=PA368.
- ↑ "Contraceptive efficacy of testosterone-induced azoospermia in normal men. World Health Organization Task Force on methods for the regulation of male fertility". Lancet 336 (8721): 955–9. October 1990. doi:10.1016/0140-6736(90)92416-F. PMID 1977002.
- ↑ "Treatment of testosterone-induced gynecomastia with the aromatase inhibitor, anastrozole". International Journal of Impotence Research 16 (1): 95–7. February 2004. doi:10.1038/sj.ijir.3901154. PMID 14963480.
- ↑ "Testosterone in Psychiatry". Archives of General Psychiatry 57 (2): 155. 2000. doi:10.1001/archpsyc.57.2.155. ISSN 0003-990X.
- ↑ "The effect of testosterone levels on mood in men: a review". Psychosomatics 54 (6): 509–514. 2013. doi:10.1016/j.psym.2013.06.018. PMID 24016385.
- ↑ "Hormonal replacement and sexuality in men". Clinics in Endocrinology and Metabolism 11 (3): 599–623. November 1982. doi:10.1016/s0300-595x(82)80003-0. PMID 6814798.
- ↑ Androgens in Health and Disease. Springer Science & Business Media. 27 May 2003. pp. 144, 259–261, 351. ISBN 978-1-59259-388-0. https://books.google.com/books?id=vDcBCAAAQBAJ&pg=PA259. Retrieved November 18, 2016.
- ↑ 56.0 56.1 "Testosterone replacement therapy in patients with prostate cancer after radical prostatectomy". The Journal of Urology 190 (2): 639–44. Aug 2013. doi:10.1016/j.juro.2013.02.002. PMID 23395803.
- ↑ "Testosterone and Other Anabolic Androgenic Steroids (AAS): FDA Statement - Risks Associated With Abuse and Dependence". 25 October 2016. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm526151.htm.
- ↑ "Testosterone Injection". 2 August 2020. https://www.drugs.com/testosterone.html.
- ↑ "Testosterone Injection". March 15, 2019. https://medlineplus.gov/druginfo/meds/a614041.html.
- ↑ "Occurrence of Pulmonary Oil Microembolism After Testosterone Undecanoate Injection: A Postmarketing Safety Analysis". Sexual Medicine 8 (2): 237–242. June 2020. doi:10.1016/j.esxm.2020.01.009. PMID 32184081.
- ↑ "Increased risk of non-fatal myocardial infarction following testosterone therapy prescription in men". PLOS ONE 9 (1): e85805. January 2014. doi:10.1371/journal.pone.0085805. PMID 24489673. Bibcode: 2014PLoSO...985805F.
- ↑ 62.0 62.1 "Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels". JAMA 310 (17): 1829–36. Nov 2013. doi:10.1001/jama.2013.280386. PMID 24193080.
- ↑ "Adverse events associated with testosterone administration". The New England Journal of Medicine 363 (2): 109–22. 2010-07-08. doi:10.1056/NEJMoa1000485. PMID 20592293.
- ↑ Staff (January 31, 2014). "FDA evaluating risk of stroke, heart attack and death with FDA-approved testosterone products". U.S. Food and Drug Administration. https://www.fda.gov/downloads/Drugs/DrugSafety/UCM383909.pdf.
- ↑ "F.D.A. Panel Backs Limits on Testosterone Drugs". The New York Times. September 17, 2014. https://www.nytimes.com/2014/09/18/health/testosterone-drugs-fda.html.
- ↑ Staff (September 5, 2014). "FDA Panel To Review Testosterone Therapy Appropriateness and Safety". CNN News. http://ireport.cnn.com/docs/DOC-1167887.
- ↑ Staff (September 17, 2014). "Joint Meeting for Bone, Reproductive and Urologic Drugs Advisory Committee (BRUDAC) and the Drug Safety And Risk Management Advisory Committee (DSARM AC) – FDA background documents for the discussion of two major issues in testosterone replacement therapy (TRT): 1. The appropriate indicated population for TRT, and 2. The potential for adverse cardiovascular outcomes associated with use of TRT". Food and Drug Administration. https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ReproductiveHealthDrugsAdvisoryCommittee/UCM412536.pdf.
- ↑ Staff (June 19, 2014). "FDA adding general warning to testosterone products about potential for venous blood clots". https://www.fda.gov/Drugs/DrugSafety/ucm401746.htm.
- ↑ "Testosterone and cardiovascular risk in men: a systematic review and meta-analysis of randomized placebo-controlled trials". Mayo Clinic Proceedings 82 (1): 29–39. Jan 2007. doi:10.4065/82.1.29. PMID 17285783.
- ↑ "Clinical review 1: Adverse effects of testosterone therapy in adult men: a systematic review and meta-analysis". The Journal of Clinical Endocrinology and Metabolism 95 (6): 2560–75. Jun 2010. doi:10.1210/jc.2009-2575. PMID 20525906.
- ↑ "Testosterone Products: Drug Safety Communication – FDA Investigating Risk of Cardiovascular Events". FDA. January 31, 2014. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm384225.htm.
- ↑ "Research provides reassurance about the safety of testosterone treatment". NIHR Evidence (National Institute for Health and Care Research). 6 February 2023. doi:10.3310/nihrevidence_56696. https://evidence.nihr.ac.uk/alert/research-provides-reassurance-about-safety-testosterone-treatment/.
- ↑ "Adverse cardiovascular events and mortality in men during testosterone treatment: an individual patient and aggregate data meta-analysis". The Lancet. Healthy Longevity 3 (6): e381–e393. June 2022. doi:10.1016/S2666-7568(22)00096-4. PMID 35711614.
- ↑ "Testosterone therapy and prostate carcinoma". Current Urology Reports 10 (6): 453–59. Nov 2009. doi:10.1007/s11934-009-0072-1. PMID 19863857.
- ↑ "Prostate cancer in men using testosterone supplementation". The Journal of Urology 174 (2): 534–38; discussion 538. Aug 2005. doi:10.1097/01.ju.0000165166.36280.60. PMID 16006887.
- ↑ 76.0 76.1 "Population differences in the testosterone levels of young men are associated with prostate cancer disparities in older men". American Journal of Human Biology 22 (4): 449–455. 2010. doi:10.1002/ajhb.21016. PMID 20087895.
- ↑ "Human prostate cancer risk factors". Cancer 101 (10 Suppl): 2371–2490. Nov 2004. doi:10.1002/cncr.20408. PMID 15495199.
- ↑ "Testosterone Pregnancy and Breastfeeding Warnings". https://www.drugs.com/pregnancy/testosterone.html.
- ↑ 79.0 79.1 79.2 Endocrinology Adult and Pediatric: Reproductive Endocrinology. Elsevier Health Sciences. 7 May 2013. pp. 1–. ISBN 978-0-323-22152-8. https://books.google.com/books?id=Np8xxP6pcdUC&pg=RA1-PT1157.
- ↑ 80.0 80.1 Hair Growth and Disorders. Springer Science & Business Media. 26 June 2008. pp. 182–. ISBN 978-3-540-46911-7. https://books.google.com/books?id=pHrX2-huQCoC&pg=PA182.
- ↑ 81.0 81.1 Androgens in Health and Disease. Springer Science & Business Media. 27 May 2003. pp. 78–. ISBN 978-1-59259-388-0. https://books.google.com/books?id=vDcBCAAAQBAJ&pg=PA78. Retrieved December 6, 2016.
- ↑ Hypospadias and Genital Development. Springer Science & Business Media. 6 December 2012. pp. 37–. ISBN 978-1-4419-8995-6. https://books.google.com/books?id=8zfaBwAAQBAJ&pg=PA37. Retrieved December 6, 2016.
- ↑ Neurosteroids. Frontiers E-books. pp. 357–358. ISBN 978-2-88919-078-2. https://books.google.com/books?id=fSgNRlZUwt0C&pg=PA358. Retrieved December 6, 2016.
- ↑ "Sources of estrogen and their importance". J. Steroid Biochem. Mol. Biol. 86 (3–5): 225–30. September 2003. doi:10.1016/S0960-0760(03)00360-1. PMID 14623515.
- ↑ Andrology: Male Reproductive Health and Dysfunction (3rd ed.). Berlin: Springer. 2009. p. 459. ISBN 978-3-540-78354-1.
- ↑ Brody's Human Pharmacology. Elsevier Health Sciences. 1 April 2009. pp. 468–469. ISBN 978-0-323-07575-6. https://books.google.com/books?id=kfsrz_-OrMQC&pg=PA468. Retrieved November 13, 2016.
- ↑ 87.0 87.1 87.2 87.3 Cite error: Invalid
<ref>tag; no text was provided for refs namedBecker2001 - ↑ Campbell-Walsh Urology. Elsevier Health Sciences. 23 October 2015. pp. 7207–. ISBN 978-0-323-26374-0. https://books.google.com/books?id=OH_OCgAAQBAJ&pg=PT7207. Retrieved December 6, 2016.
- ↑ 89.0 89.1 "Pharmacology of anabolic steroids". British Journal of Pharmacology 154 (3): 502–21. June 2008. doi:10.1038/bjp.2008.165. PMID 18500378.
- ↑ 90.0 90.1 Tietz Textbook of Clinical Chemistry and Molecular Diagnostics. Elsevier Health Sciences. 14 October 2012. pp. 1947–. ISBN 978-1-4557-5942-2. https://books.google.com/books?id=BBLRUI4aHhkC&pg=PA1947.
- ↑ 91.0 91.1 "Dissociating Behavioral, Autonomic, and Neuroendocrine Effects of Androgen Steroids in Animal Models". Psychiatric Disorders. Methods in Molecular Biology. 829. Springer. 2012. pp. 397–431. doi:10.1007/978-1-61779-458-2_26. ISBN 978-1-61779-457-5.
- ↑ 92.0 92.1 Andrology: Male Reproductive Health and Dysfunction. Springer Science & Business Media. 13 January 2010. pp. 49–54,441–446. ISBN 978-3-540-78355-8. https://books.google.com/books?id=mEgckDNkonUC&pg=PA442.
- ↑ Yen & Jaffe's Reproductive Endocrinology E-Book: Physiology, Pathophysiology, and Clinical Management. Elsevier Health Sciences. 23 December 2017. pp. 292–. ISBN 978-0-323-58232-2. https://books.google.com/books?id=67ZEDwAAQBAJ&pg=PA292. Retrieved March 31, 2018.
- ↑ 94.0 94.1 94.2 "Testosterone preparations for clinical use in males". Testosterone: Action, Deficiency, Substitution. Cambridge University Press. 26 July 2012. pp. 309–335. doi:10.1017/CBO9781139003353.016. ISBN 978-1-107-01290-5.
- ↑ 95.0 95.1 95.2 95.3 95.4 95.5 The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. 14 November 2014. pp. 641–642. ISBN 978-1-4757-2085-3. https://books.google.com/books?id=0vXTBwAAQBAJ&pg=PA641.
- ↑ Endocrinology: Adult and Pediatric. Elsevier Health Sciences. 25 February 2015. pp. 2387–. ISBN 978-0-323-32195-2. https://books.google.com/books?id=xmLeBgAAQBAJ&pg=PA2387. Retrieved November 18, 2016.
- ↑ Practical Urology: Essential Principles and Practice: Essential Principles and Practice. Springer Science & Business Media. 10 May 2011. pp. 228–. ISBN 978-1-84882-034-0. https://books.google.com/books?id=A9m8TkdCUqEC&pg=PA228. Retrieved November 18, 2016.
- ↑ 98.0 98.1 98.2 Essentials of Strength Training and Conditioning (4th ed.). Human Kinetics. 23 September 2015. pp. 229, 233. ISBN 978-1-4925-0162-6. https://books.google.com/books?id=bfuXCgAAQBAJ&pg=PA233. Retrieved November 18, 2016.
- ↑ Anabolic Steroids and the Athlete (2nd ed.). McFarland. 16 January 2002. pp. 180–. ISBN 978-0-7864-1128-3. https://books.google.com/books?id=OGcQ0Tp2AFcC&pg=PA180. Retrieved November 13, 2016.
- ↑ 100.0 100.1 100.2 100.3 100.4 Testosterone Dreams: Rejuvenation, Aphrodisia, Doping. University of California Press. 21 February 2005. pp. 134–. ISBN 978-0-520-93978-3. https://archive.org/details/testosteronedrea00hobe.
- ↑ The Scientific Basis of Urology. CRC Press. 26 July 2010. pp. 294–. ISBN 978-1-84184-749-8. https://books.google.com/books?id=h6HSBQAAQBAJ&pg=PA294. Retrieved November 18, 2016.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedMelmedPolonsky2015 - ↑ "Testosterone Undecanoate—Schering AG". Drugs 5 (6): 368–369. 2004. doi:10.2165/00126839-200405060-00012. PMID 15563244.
- ↑ "The History of Testosterone and the Testes: From Antiquity to Modern Times". Testosterone. Springer. 2017. pp. 1–19. doi:10.1007/978-3-319-46086-4_1. ISBN 978-3-319-46084-0.
- ↑ "ENDOCRINE HISTORY: The history of discovery, synthesis and development of testosterone for clinical use". European Journal of Endocrinology 180 (6): R201–R212. June 2019. doi:10.1530/EJE-19-0071. PMID 30959485.
- ↑ "Testosterone deficiency: a historical perspective". Asian Journal of Andrology 16 (2): 161–8. 2014. doi:10.4103/1008-682X.122358. PMID 24435052.
- ↑ "The History of Testosterone and the Evolution of its Therapeutic Potential". Sexual Medicine Reviews 8 (2): 286–296. April 2020. doi:10.1016/j.sxmr.2018.03.002. PMID 29661690.
- ↑ "Male Menopause". NHS Choices. April 8, 2016. http://www.nhs.uk/conditions/Male-menopause/Pages/Introduction.aspx.
- ↑ ""Low T": The triumph of marketing over science « Science-Based Medicine". Science-Based Medicine. November 25, 2013. https://www.sciencebasedmedicine.org/low-t-the-triumph-of-marketing-over-science/.
- ↑ 110.0 110.1 110.2 "Disease mongering of age-associated declines in testosterone and growth hormone levels". Journal of the American Geriatrics Society 63 (4): 809–11. April 2015. doi:10.1111/jgs.13391. PMID 25809947.
- ↑ 111.0 111.1 111.2 111.3 111.4 "Testosterone - International". Drugs.com. https://www.drugs.com/international/testosterone.html.
- ↑ 112.0 112.1 Index Nominum 2000: International Drug Directory. Taylor & Francis. January 2000. ISBN 978-3-88763-075-1. https://books.google.com/books?id=5GpcTQD_L2oC. Retrieved December 2, 2016.
- ↑ Владимир Мюллер (15 April 2016). Англо-русский словарь. Русско-английский словарь. 250 000 слов. ЛитРес. pp. 643–. ISBN 978-5-457-98308-3. https://books.google.com/books?id=rOP6CwAAQBAJ&pg=PA643. Retrieved December 2, 2016.
- ↑ 114.0 114.1 114.2 114.3 114.4 Cite error: Invalid
<ref>tag; no text was provided for refs namedDrugs@FDA - ↑ Endocrinology of Aging. 34. Springer Science & Business Media. 5 November 1999. 141–. doi:10.1016/s0011-5029(98)90024-4. ISBN 978-1-59259-715-4. https://books.google.com/books?id=hGD0BwAAQBAJ&pg=PA141. Retrieved November 15, 2016.
- ↑ Androgens in Health and Disease. Springer Science & Business Media. 27 May 2003. ISBN 978-1-59259-388-0. https://books.google.com/books?id=vDcBCAAAQBAJ&pg=PA259. Retrieved November 18, 2016.
- ↑ 117.0 117.1 117.2 "Drug Product Database - Health Canada". Health Canada. 2010-03-18. http://www.hc-sc.gc.ca/dhp-mps/prodpharma/databasdon/index-eng.php.
- ↑ Drug Abuse Handbook, Second Edition. CRC Press. 21 December 2006. pp. 30–. ISBN 978-1-4200-0346-8. https://books.google.com/books?id=ZjrMBQAAQBAJ&pg=PA30. Retrieved November 11, 2017.
- ↑ Pharmacology for Canadian Health Care Practice. Elsevier Health Sciences. 5 August 2016. pp. 50–. ISBN 978-1-77172-066-3. https://books.google.com/books?id=dNgoDwAAQBAJ&pg=PA50. Retrieved November 11, 2017.
- ↑ "Impact of exogenous testosterone on mood: a systematic review and meta-analysis of randomized placebo-controlled trials". Annals of Clinical Psychiatry 26 (1): 19–32. Feb 2014. PMID 24501728. http://www.aacp.com/pdf%2F0214%2F0214ACP%5FAmanatkar%2Epdf.[yes|permanent dead link|dead link}}]
- ↑ "Testosterone and depression: systematic review and meta-analysis". J Psychiatr Pract 15 (4): 289–305. July 2009. doi:10.1097/01.pra.0000358315.88931.fc. PMID 19625884.
- ↑ 122.0 122.1 "Will testosterone replacement therapy become a new treatment of chronic heart failure? A review based on 8 clinical trials". Journal of Thoracic Disease 8 (5): E269–77. May 2016. doi:10.21037/jtd.2016.03.39. PMID 27162680.
- ↑ 123.0 123.1 "Testosterone Supplementation in Heart Failure: A Meta-Analysis". Circulation: Heart Failure 5 (3): 315–21. May 2012. doi:10.1161/CIRCHEARTFAILURE.111.965632. PMID 22511747.
- ↑ "Male Hormonal Contraception: Where Are We Now?". Current Obstetrics and Gynecology Reports 5: 38–47. 2016. doi:10.1007/s13669-016-0140-8. PMID 26949570.
- ↑ "The current state of male hormonal contraception". Pharmacology & Therapeutics 163: 109–17. July 2016. doi:10.1016/j.pharmthera.2016.03.012. PMID 27016468.
- ↑ "Testosterone intranasal (low-dose)". http://adisinsight.springer.com/drugs/800029680.
- ↑ "The dark side of testosterone deficiency: II. Type 2 diabetes and insulin resistance". Journal of Andrology 30 (1): 23–32. 2009. doi:10.2164/jandrol.108.005751. PMID 18772488.
- ↑ "Androgens, aging, and Alzheimer's disease". Endocrine 29 (2): 233–41. Apr 2006. doi:10.1385/ENDO:29:2:233. PMID 16785599.
- ↑ "Age-related testosterone depletion and the development of Alzheimer disease". JAMA 292 (12): 1431–32. Sep 2004. doi:10.1001/jama.292.12.1431-b. PMID 15383512.
- ↑ "Current concepts in aesthetic endocrinology". Gynecol. Endocrinol. 16 (6): 431–41. December 2002. doi:10.1080/gye.16.6.431.441. PMID 12626029.
Further reading
- Andrology: Male Reproductive Health and Dysfunction. Springer Science & Business Media. 13 January 2010. ISBN 978-3-540-78355-8. https://books.google.com/books?id=mEgckDNkonUC. Retrieved November 13, 2016.
- Testosterone: Action, Deficiency, Substitution. Cambridge University Press. 26 July 2012. ISBN 978-1-107-01290-5. https://books.google.com/books?id=MkrAPaQ4wJkC. Retrieved July 31, 2018.
- Testosterone: From Basic to Clinical Aspects. Springer. 30 March 2017. ISBN 978-3-319-46086-4. https://books.google.com/books?id=Et6TDgAAQBAJ. Retrieved July 31, 2018.
- "Testosterone deficiency: a historical perspective". Asian J. Androl. 16 (2): 161–8. 2014. doi:10.4103/1008-682X.122358. PMID 24435052.
- Anabolics. Molecular Nutrition Llc. 2011. ISBN 978-0-9828280-1-4. https://books.google.com/books?id=afKLA-6wW0oC. Retrieved November 18, 2016.
- "Pharmacology of testosterone replacement therapy preparations". Translational Andrology and Urology 5 (6): 834–843. December 2016. doi:10.21037/tau.2016.07.10. PMID 28078214.
- "On the effects of testosterone on brain behavioral functions". Frontiers in Neuroscience 9: 12. February 2015. doi:10.3389/fnins.2015.00012. PMID 25741229.
External links
- "Testosterone". Drug Information Portal. U.S. National Library of Medicine. https://druginfo.nlm.nih.gov/drugportal/name/testosterone.
- "Testosterone Transdermal Patch". https://medlineplus.gov/druginfo/meds/a601118.html.
- "Testosterone Buccal". https://medlineplus.gov/druginfo/meds/a603034.html.
- "Testosterone Topical". https://medlineplus.gov/druginfo/meds/a605020.html.
- "Testosterone Injection". https://medlineplus.gov/druginfo/meds/a614041.html.
- "Testosterone Nasal Gel". https://medlineplus.gov/druginfo/meds/a615025.html.
{{Navbox
| name = Androgens and antiandrogens | title = Androgens and antiandrogens | state = collapsed | listclass = hlist | groupstyle = text-align:center;
| group1 = Androgens
(incl. AAS)
| list1 =
| group2 = Antiandrogens | list2 = {{Navbox|child | groupstyle = text-align:center; | groupwidth = 9em;
| group1 = AR antagonists | list1 =
- Steroidal: Abiraterone acetate
- Canrenone
- Chlormadinone acetate
- Cyproterone acetate
- Delmadinone acetate
- Dienogest
- Drospirenone
- Medrogestone
- Megestrol acetate
- Nomegestrol acetate
- Osaterone acetate
- Oxendolone
- Potassium canrenoate
- Spironolactone
- Nonsteroidal: Apalutamide
- Bicalutamide
- Cimetidine
- Darolutamide
- Enzalutamide
- Flutamide
- Ketoconazole
- Nilutamide
- Seviteronel†
- Topilutamide (fluridil)
| group2 = Steroidogenesis| list2 =
inhibitors
| 5α-Reductase | |
|---|---|
| Others |
| group3 = Antigonadotropins | list3 =
- D2 receptor antagonists (prolactin releasers) (e.g., domperidone, metoclopramide, risperidone, haloperidol, chlorpromazine, sulpiride)
- Estrogens (e.g., bifluranol, [[diethylstilbestrol, estradiol, estradiol esters, ethinylestradiol, ethinylestradiol sulfonate, paroxypropione)
- GnRH agonists (e.g., leuprorelin)
- GnRH antagonists (e.g., cetrorelix)
- Progestogens (incl., chlormadinone acetate, [[cyproterone acetate, hydroxyprogesterone caproate, gestonorone caproate, [[Chemistry:Medroxyprogesterone medroxyprogesterone acetate, Chemistry:Megestrol acetate|megestrol acetate]])
| group4 = Others | list4 =
- Androstenedione immunogens: Androvax (androstenedione albumin)
- Ovandrotone albumin (Fecundin)
}}
| liststyle = background:#DDDDFF;| list3 =
- #WHO-EM
- ‡Withdrawn from market
- Clinical trials:
- †Phase III
- §Never to phase III
- See also
- Androgen receptor modulators
- Estrogens and antiestrogens
- Progestogens and antiprogestogens
- List of androgens/anabolic steroids
}}
 |



