Medicine:Toxoplasmosis
| Toxoplasmosis | |
|---|---|
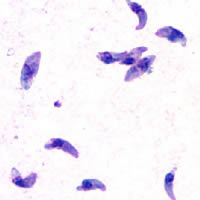 | |
| T. gondii tachyzoites | |
| Specialty | Infectious disease |
| Symptoms | Often none, during pregnancy (birth defects)[1][2] |
| Causes | Toxoplasma gondii[3] |
| Risk factors | Eating poorly cooked food, exposure to infected cat feces[3] |
| Diagnostic method | Blood test, amniotic fluid test[4] |
| Treatment | During pregnancy spiramycin or pyrimethamine/sulfadiazine and folinic acid[5] |
| Frequency | Up to 50% of people, 200,000 cases of congenital toxoplasmosis a year[6][7] |
Toxoplasmosis is a parasitic disease caused by Toxoplasma gondii, an apicomplexan.[3] Infections with toxoplasmosis are associated with a variety of neuropsychiatric and behavioral conditions.[8] Occasionally, people may have a few weeks or months of mild, flu-like illness such as muscle aches and tender lymph nodes.[1] In a small number of people, eye problems may develop.[1] In those with a weak immune system, severe symptoms such as seizures and poor coordination may occur.[1] If a woman becomes infected during pregnancy, a condition known as congenital toxoplasmosis may affect the child.[1]
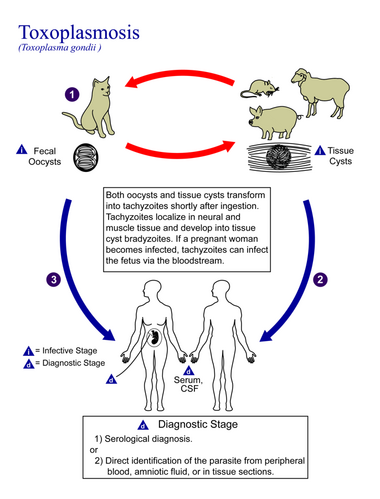
Toxoplasmosis is usually spread by eating poorly cooked food that contains cysts, exposure to infected cat feces, and from an infected woman to her baby during pregnancy.[3] Rarely, the disease may be spread by blood transfusion.[3] It is not otherwise spread between people.[3] The parasite is known to reproduce sexually only in the cat family.[9] However, it can infect most types of warm-blooded animals, including humans.[9] Diagnosis is typically by testing blood for antibodies or by testing the amniotic fluid in a pregnant patient for the parasite's DNA.[4]
Prevention is by properly preparing and cooking food.[10] Pregnant women are also recommended not to clean cat litter boxes or, if they must, to wear gloves and wash their hands afterwards.[10] Treatment of otherwise healthy people is usually not needed.[5] During pregnancy, spiramycin or pyrimethamine/sulfadiazine and folinic acid may be used for treatment.[5]
Up to half of the world's population is infected by T. gondii, but have no symptoms.[7] In the United States, approximately 11% of people have been infected, while in some areas of the world this is more than 60%.[3] Approximately 200,000 cases of congenital toxoplasmosis occur a year.[6] Charles Nicolle and Louis Manceaux first described the organism in 1908.[11] In 1941, transmission during pregnancy from a pregnant woman to her baby was confirmed.[11] There is tentative evidence that infection may affect people's behavior.[12]
Signs and symptoms
Infection has three stages:
Acute
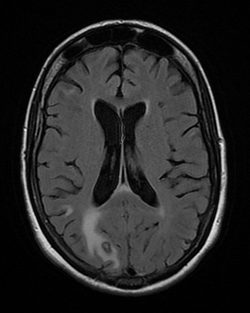
Acute toxoplasmosis is often asymptomatic in healthy adults.[13][14] However, symptoms may manifest and are often influenza-like: swollen lymph nodes, headaches, fever, and fatigue,[15] or muscle aches and pains that last for a month or more. It is rare for a human with a fully functioning immune system to develop severe symptoms following infection. People with weakened immune systems are likely to experience headache, confusion, poor coordination, seizures, lung problems that may resemble tuberculosis or Pneumocystis jirovecii pneumonia (a common opportunistic infection that occurs in people with AIDS), or chorioretinitis caused by severe inflammation of the retina (ocular toxoplasmosis).[15] Young children and immunocompromised people, such as those with HIV/AIDS, those taking certain types of chemotherapy, or those who have recently received an organ transplant, may develop severe toxoplasmosis. This can cause damage to the brain (encephalitis) or the eyes (necrotizing retinochoroiditis).[16] Infants infected via placental transmission may be born with either of these problems, or with nasal malformations, although these complications are rare in newborns. The toxoplasmic trophozoites causing acute toxoplasmosis are referred to as tachyzoites, and are typically found in various tissues and body fluids, but rarely in blood or cerebrospinal fluid.[17]
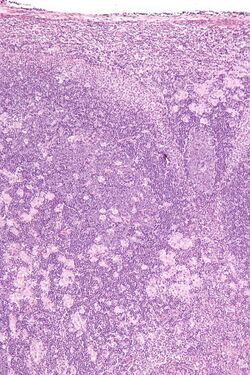
Swollen lymph nodes are commonly found in the neck or under the chin, followed by the armpits and the groin. Swelling may occur at different times after the initial infection, persist, and recur for various times independently of antiparasitic treatment.[18] It is usually found at single sites in adults, but in children, multiple sites may be more common. Enlarged lymph nodes will resolve within 1–2 months in 60% of cases. However, a quarter of those affected take 2–4 months to return to normal, and 8% take 4–6 months. A substantial number (6%) do not return to normal until much later.[19]
Latent
Due to the absence of obvious symptoms,[13][14] hosts easily become infected with T. gondii and develop toxoplasmosis without knowing it. Although mild, flu-like symptoms occasionally occur during the first few weeks following exposure, infection with T. gondii produces no readily observable symptoms in healthy human adults.[7][20] In most immunocompetent people, the infection enters a latent phase, during which only bradyzoites (in tissue cysts) are present;[21] these tissue cysts and even lesions can occur in the retinas, alveolar lining of the lungs (where an acute infection may mimic a Pneumocystis jirovecii infection), heart, skeletal muscle, and the central nervous system (CNS), including the brain.[22] Cysts form in the CNS (brain tissue) upon infection with T. gondii and persist for the lifetime of the host.[23] Most infants who are infected while in the womb have no symptoms at birth, but may develop symptoms later in life.[24]
Reviews of serological studies have estimated that 30–50% of the global population has been exposed to and may be chronically infected with latent toxoplasmosis, although infection rates differ significantly from country to country.[7][25][26] This latent state of infection has recently been associated with numerous disease burdens,[7] neural alterations,[23][25] and subtle gender-dependent behavioral changes in immunocompetent humans,[27][28] as well as an increased risk of motor vehicle collisions.[29]
Skin
While rare, skin lesions may occur in the acquired form of the disease, including roseola and erythema multiforme-like eruptions, prurigo-like nodules, urticaria, and maculopapular lesions. Newborns may have punctate macules, ecchymoses, or "blueberry muffin" lesions. Diagnosis of cutaneous toxoplasmosis is based on the tachyzoite form of T. gondii being found in the epidermis.[30] It is found in all levels of the epidermis, is about 6 by 2 μm and bow-shaped, with the nucleus being one-third of its size. It can be identified by electron microscopy or by Giemsa staining tissue where the cytoplasm shows blue, the nucleus red.[31]
Cause
Parasitology
In its lifecycle, T. gondii adopts several forms.[32] Tachyzoites are responsible for acute infection; they divide rapidly and spread through the tissues of the body. Tachyzoites are also known as "tachyzoic merozoites", a descriptive term that conveys more precisely the parasitological nature of this stage.[33] After proliferating, tachyzoites convert into bradyzoites, which are inside latent intracellular tissue cysts that form mainly in the muscles and brain. The formation of cysts is in part triggered by the pressure of the host immune system.[34] The bradyzoites (also called "bradyzoic merozoites") are not responsive to antibiotics. Bradyzoites, once formed, can remain in the tissues for the lifespan of the host. In a healthy host, if some bradyzoites convert back into active tachyzoites, the immune system will quickly destroy them. However, in immunocompromised individuals, or in fetuses, which lack a developed immune system, the tachyzoites can run rampant and cause significant neurological damage.[32]
The parasite's survival is dependent on a balance between host survival and parasite proliferation.[34] T. gondii achieves this balance by manipulating the host's immune response, reducing the host's immune response, and enhancing the parasite's reproductive advantage.[34] Once it infects a normal host cell, it resists damage caused by the host's immune system, and changes the host's immune processes.[35] As it forces its way into the host cell, the parasite forms a parasitophorous vacuole (PV) membrane from the membrane of the host cell.[2][36] The PV encapsulates the parasite, and is both resistant to the activity of the endolysosomal system, and can take control of the host's mitochondria and endoplasmic reticulum.[2][36]
When first invading the cell, the parasite releases ROP proteins from the bulb of the rhoptry organelle.[2] These proteins translocate to the nucleus and the surface of the PV membrane where they can activate STAT pathways to modulate the expression of cytokines at the transcriptional level, bind and inactivate PV membrane destroying IRG proteins, among other possible effects.[2][36][37] Additionally, certain strains of T. gondii can secrete a protein known as GRA15, activating the NF-κB pathway, which upregulates the pro-inflammatory cytokine IL-12 in the early immune response, possibly leading to the parasite's latent phase.[2] The parasite's ability to secrete these proteins depends on its genotype and affects its virulence.[2][37]
The parasite also influences an anti-apoptotic mechanism, allowing the infected host cells to persist and replicate. One method of apoptosis resistance is by disrupting pro-apoptosis effector proteins, such as BAX and BAK.[38] To disrupt these proteins, T. gondii causes conformational changes to the proteins, which prevent the proteins from being transported to various cellular compartments where they initiate apoptosis events. T. gondii does not, however, cause downregulation of the pro-apoptosis effector proteins.[38]
T. gondii also has the ability to initiate autophagy of the host's cells.[39] This leads to a decrease in healthy, uninfected cells, and consequently fewer host cells to attack the infected cells. Research by Wang et al finds that infected cells lead to higher levels of autophagosomes in normal and infected cells.[39] Their research reveals that T. gondii causes host cell autophagy using a calcium-dependent pathway.[39] Another study suggests that the parasite can directly affect calcium being released from calcium stores, which are important for the signalling processes of cells.[38]
The mechanisms above allow T. gondii to persist in a host. Some limiting factors for the toxoplasma is that its influence on the host cells is stronger in a weak immune system and is quantity-dependent, so a large number of T. gondii per host cell cause a more severe effect.[40] The effect on the host also depends on the strength of the host immune system. Immunocompetent individuals do not normally show severe symptoms or any at all, while fatality or severe complications can result in immunocompromised individuals.[40]
T. gondii has been shown to produce a protein called GRA28, released by the MYR1 secretory pathway, which interferes with gene expression in infected cells and results in cells that behave like dendritic cells, becoming highly mobile in the body.[41]
Since the parasite can change the host's immune response, it may also have an effect, positive or negative, on the immune response to other pathogenic threats.[34] This includes, but is not limited to, the responses to infections by Helicobacter felis, Leishmania major, or other parasites, such as Nippostrongylus brasiliensis.[34]
Transmission
Toxoplasmosis is generally transmitted through the mouth when Toxoplasma gondii oocysts or tissue cysts are accidentally eaten.[42] Congenital transmittance from mother to fetus can also occur.[43] Transmission may also occur during the solid organ transplant process[44] or hematogenous stem cell transplants.[45]
Oral transmission may occur through:
- Ingestion of raw or partly cooked meat, especially pork, lamb, or venison containing Toxoplasma cysts: Infection prevalence in countries where undercooked meat is traditionally eaten has been related to this transmission method. Tissue cysts may also be ingested during hand-to-mouth contact after handling undercooked meat, or from using knives, utensils, or cutting boards contaminated by raw meat.[46]
- Ingestion of unwashed fruit or vegetables that have been in contact with contaminated soil containing infected cat feces.[47]
- Ingestion of cat feces containing oocysts: This can occur through hand-to-mouth contact following gardening, cleaning a cat's litter box, contact with children's sandpits; the parasite can survive in the environment for months.[48]
- Ingestion of untreated, unfiltered water through direct consumption or utilization of water for food preparation.[49]
- Ingestion of unpasteurized milk and milk products, particularly goat's milk.[50]
- Ingestion of raw seafood.[51]
Cats excrete the pathogen in their feces for a number of weeks after contracting the disease, generally by eating an infected intermediate host that could include mammals (like rodents) or birds. Oocyst shedding usually starts from the third day after ingestion of infected intermediate hosts, and may continue for weeks. The oocysts are not infective when excreted. After about a day, the oocyst undergoes a process called sporulation and becomes potentially pathogenic.[52] In addition to cats, birds and mammals including human beings are also intermediate hosts of the parasite and are involved in the transmission process. However the pathogenicity varies with the age and species involved in infection and the mode of transmission of T. gondii.[53]
Toxoplasmosis may also be transmitted through solid organ transplants. Toxoplasma-seronegative recipients who receive organs from recently infected Toxoplasma-seropositive donors are at risk. Organ recipients who have latent toxoplasmosis are at risk of the disease reactivating in their system due to the immunosuppression occurring during solid organ transplant.[44] Recipients of hematogenous stem cell transplants may experience higher risk of infection due to longer periods of immunosuppression.[45]
Heart and lung transplants provide the highest risk for toxoplasmosis infection due to the striated muscle making up the heart,[44] which can contain cysts, and risks for other organs and tissues vary widely.[54] Risk of transmission can be reduced by screening donors and recipients prior to the transplant procedure and providing treatment.[54]
Pregnancy precautions
Congenital toxoplasmosis is a specific form of toxoplasmosis in which an unborn fetus is infected via the placenta.[55] Congenital toxoplasmosis is associated with fetal death and miscarriage, and in infants, it is associated with hydrocephalus, cerebral calcifications and chorioretinitis, leading to encephalopathy and possibly blindness.[6] If a woman receives her first exposure to T. gondii while pregnant, the fetus is at particular risk.[6] A simple blood draw at the first prenatal doctor visit can determine whether or not a woman has had previous exposure and therefore whether or not she is at risk. A positive antibody titer indicates previous exposure and immunity, and largely ensures the unborn fetus' safety.
Not much evidence exists around the effect of education before pregnancy to prevent congenital toxoplasmosis.[56] However educating parents before the baby is born has been suggested to be effective because it may improve food, personal and pet hygiene.[56] More research is needed to find whether antenatal education can reduce congenital toxoplasmosis.[56]
For pregnant women with negative antibody titers, indicating no previous exposure to T. gondii, serology testing as frequent as monthly is advisable as treatment during pregnancy for those women exposed to T. gondii for the first time dramatically decreases the risk of passing the parasite to the fetus. Since a baby's immune system does not develop fully for the first year of life, and the resilient cysts that form throughout the body are very difficult to eradicate with antiprotozoans, an infection can be very serious in the young.[citation needed]
Despite these risks, pregnant women are not routinely screened for toxoplasmosis in most countries, for reasons of cost-effectiveness and the high number of false positives generated; Portugal,[57] France ,[58] Austria,[58] Uruguay,[59] and Italy[60] are notable exceptions, and some regional screening programmes operate in Germany , Switzerland and Belgium.[60] As invasive prenatal testing incurs some risk to the fetus (18.5 pregnancy losses per toxoplasmosis case prevented),[58] postnatal or neonatal screening is preferred. The exceptions are cases where fetal abnormalities are noted, and thus screening can be targeted.[58]
Pregnant women should avoid handling raw meat, drinking raw milk (especially goat milk) and be advised to not eat raw or undercooked meat regardless of type.[61] Because of the obvious relationship between Toxoplasma and cats it is also often advised to avoid exposure to cat feces, and refrain from gardening (cat feces are common in garden soil) or at least wear gloves when so engaged.[61] Most cats are not actively shedding oocysts, since they get infected in the first six months of their life, when they shed oocysts for a short period of time (1–2 weeks.)[62] However, these oocysts get buried in the soil, sporulate and remain infectious for periods ranging from several months to more than a year.[61] Numerous studies have shown living in a household with a cat is not a significant risk factor for T. gondii infection,[61][63][64] though living with several kittens has some significance.[65]
In 2006, a Czech research team[66] discovered women with high levels of toxoplasmosis antibodies were significantly more likely to give birth to baby boys than baby girls. In most populations, the birth rate is around 51% boys, but people infected with T. gondii had up to a 72% chance of a boy.[67]
Diagnosis
Diagnosis of toxoplasmosis in humans is made by biological, serological, histological, or molecular methods, or by some combination of the above.[62] Toxoplasmosis can be difficult to distinguish from primary central nervous system lymphoma. It mimics several other infectious diseases so clinical signs are non-specific and are not sufficiently characteristic for a definite diagnosis. As a result, the possibility of an alternative diagnosis is supported by a failed trial of antimicrobial therapy (pyrimethamine, sulfadiazine, and folinic acid (USAN: leucovorin)), i.e., if the drugs produce no effect clinically and no improvement on repeat imaging.[citation needed]
T. gondii may also be detected in blood, amniotic fluid, or cerebrospinal fluid by using polymerase chain reaction.[68] T. gondii may exist in a host as an inactive cyst that would likely evade detection.[citation needed]
Serological testing can detect T. gondii antibodies in blood serum, using methods including the Sabin–Feldman dye test (DT), the indirect hemagglutination assay, the indirect fluorescent antibody assay (IFA), the direct agglutination test, the latex agglutination test (LAT), the enzyme-linked immunosorbent assay (ELISA), and the immunosorbent agglutination assay test (IAAT).[62]
The most commonly used tests to measure IgG antibody are the DT, the ELISA, the IFA, and the modified direct agglutination test.[69] IgG antibodies usually appear within a week or two of infection, peak within one to two months, then decline at various rates.[69] Toxoplasma IgG antibodies generally persist for life, and therefore may be present in the bloodstream as a result of either current or previous infection.[70]
To some extent, acute toxoplasmosis infections can be differentiated from chronic infections using an IgG avidity test, which is a variation on the ELISA. In the first response to infection, toxoplasma-specific IgG has a low affinity for the toxoplasma antigen; in the following weeks and month, IgG affinity for the antigen increases. Based on the IgG avidity test, if the IgG in the infected individual has a high affinity, it means that the infection began three to five months before testing. This is particularly useful in congenital infection, where pregnancy status and gestational age at time of infection determines treatment.[71]
In contrast to IgG, IgM antibodies can be used to detect acute infection but generally not chronic infection.[70] The IgM antibodies appear sooner after infection than the IgG antibodies and disappear faster than IgG antibodies after recovery.[62] In most cases, T. gondii-specific IgM antibodies can first be detected approximately a week after acquiring primary infection and decrease within one to six months; 25% of those infected are negative for T. gondii-specific IgM within seven months.[70] However, IgM may be detectable months or years after infection, during the chronic phase, and false positives for acute infection are possible.[69] The most commonly used tests for the measurement of IgM antibody are double-sandwich IgM-ELISA, the IFA test, and the immunosorbent agglutination assay (IgM-ISAGA). Commercial test kits often have low specificity, and the reported results are frequently misinterpreted.[69]
In 2021, twenty commercial anti-Toxoplasma IgG assays were evaluated in a systematic review, in comparison with an accepted reference method.[72] Most of them were enzyme-immunoassays, followed by agglutination tests, immunochromatographic tests, and a Western-Blot assay. The mean sensitivity of IgG assays ranged from 89.7% to 100% for standard titers and from 13.4% to 99.2% for low IgG titers. A few studies pointed out the ability of some methods, especially WB to detect IgG early after primary infection. The specificity of IgG assays was generally high, ranging from 91.3% to 100%; and higher than 99% for most EIA assays. The positive predictive value (PPV) was not a discriminant indicator among methods, whereas significant disparities (87.5%–100%) were reported among negative predictive values (NPV), a key-parameter assessing the ability to definitively rule out a Toxoplasma infection in patients at-risk for opportunistic infections.[72]
Congenital
Recommendations for the diagnosis of congenital toxoplasmosis include: prenatal diagnosis based on testing of amniotic fluid and ultrasound examinations; neonatal diagnosis based on molecular testing of placenta and cord blood and comparative mother-child serologic tests and a clinical examination at birth; and early childhood diagnosis based on neurologic and ophthalmologic examinations and a serologic survey during the first year of life.[55] During pregnancy, serological testing is recommended at three week intervals.[73]
Even though diagnosis of toxoplasmosis heavily relies on serological detection of specific anti-Toxoplasma immunoglobulin, serological testing has limitations. For example, it may fail to detect the active phase of T. gondii infection because the specific anti-Toxoplasma IgG or IgM may not be produced until after several weeks of infection. As a result, a pregnant woman might test negative during the active phase of T. gondii infection leading to undetected and therefore untreated congenital toxoplasmosis.[74] Also, the test may not detect T. gondii infections in immunocompromised patients because the titers of specific anti-Toxoplasma IgG or IgM may not rise in this type of patient.[citation needed]
Many PCR-based techniques have been developed to diagnose toxoplasmosis using clinical specimens that include amniotic fluid, blood, cerebrospinal fluid, and tissue biopsy. The most sensitive PCR-based technique is nested PCR, followed by hybridization of PCR products.[74] The major downside to these techniques is that they are time-consuming and do not provide quantitative data.[74]
Real-time PCR is useful in pathogen detection, gene expression and regulation, and allelic discrimination. This PCR technique utilizes the 5' nuclease activity of Taq DNA polymerase to cleave a nonextendible, fluorescence-labeled hybridization probe during the extension phase of PCR.[74] A second fluorescent dye, e.g., 6-carboxy-tetramethyl-rhodamine, quenches the fluorescence of the intact probe.[74] The nuclease cleavage of the hybridization probe during the PCR releases the effect of quenching resulting in an increase of fluorescence proportional to the amount of PCR product, which can be monitored by a sequence detector.[74]
Lymph nodes affected by Toxoplasma have characteristic changes, including poorly demarcated reactive germinal centers, clusters of monocytoid B cells, and scattered epithelioid histiocytes.[citation needed]
The classic triad of congenital toxoplasmosis includes: chorioretinitis, hydrocephalus, and intracranial arteriosclerosis.[75] Other consequences include sensorineural deafness, seizures, and intellectual disability.[76]
Congenital toxoplasmosis may also impact a child's hearing. Up to 30% of newborns have some degree of sensorineural hearing loss.[77] The child's communication skills may also be affected. A study published in 2010 looked at 106 patients, all of whom received toxoplasmosis treatment prior to 2.5 months. Of this group, 26.4% presented with language disorders.[78]
Treatment
Treatment is recommended for people with serious health problems, such as people with HIV whose CD4 counts are under 200 cells/mm3. Trimethoprim/sulfamethoxazole is the drug of choice to prevent toxoplasmosis, but not for treating active disease. A 2012 study shows a promising new way to treat the active and latent form of this disease using two endochin-like quinolones.[79]
Acute
The medications prescribed for acute toxoplasmosis are the following:[citation needed]
- Pyrimethamine – an antimalarial medication
- Sulfadiazine – an antibiotic used in combination with pyrimethamine to treat toxoplasmosis
- Combination therapy is usually given with folic acid supplements to reduce incidence of thrombocytopaenia.
- Combination therapy is most useful in the setting of HIV.
- Clindamycin[80]
- Spiramycin – an antibiotic used most often for pregnant women to prevent the infection of their children.
(other antibiotics, such as minocycline, have seen some use as a salvage therapy).
If infected during pregnancy, spiramycin is recommended in the first and early second trimesters while pyrimethamine/sulfadiazine and leucovorin is recommended in the late second and third trimesters.[81]
Latent
In people with latent toxoplasmosis, the cysts are immune to these treatments, as the antibiotics do not reach the bradyzoites in sufficient concentration.
The medications prescribed for latent toxoplasmosis are:
- Atovaquone – an antibiotic that has been used to kill Toxoplasma cysts inside AIDS patients[82]
- Clindamycin – an antibiotic that, in combination with atovaquone, seemed to optimally kill cysts in mice[83]
Congenital
When a pregnant woman is diagnosed with acute toxoplasmosis, amniocentesis can be used to determine whether the fetus has been infected or not. When a pregnant woman develops acute toxoplasmosis, the tachyzoites have approximately a 30% chance of entering the placental tissue, and from there entering and infecting the fetus. As gestational age at the time of infection increases, the chance of fetal infection also increases.[32]
If the parasite has not yet reached the fetus, spiramycin can help to prevent placental transmission. If the fetus has been infected, the pregnant woman can be treated with pyrimethamine and sulfadiazine, with folinic acid, after the first trimester. They are treated after the first trimester because pyrimethamine has an antifolate effect, and lack of folic acid can interfere with fetal brain formation and cause thrombocytopaenia.[84] Infection in earlier gestational stages correlates with poorer fetal and neonatal outcomes, particularly when the infection is untreated.[85]
Newborns who undergo 12 months of postnatal anti-toxoplasmosis treatment have a low chance of sensorineural hearing loss.[86] Information regarding treatment milestones for children with congenital toxoplasmosis have been created for this group.[87]
Epidemiology
T. gondii infections occur throughout the world, although infection rates differ significantly by country.[26] For women of childbearing age, a survey of 99 studies within 44 countries found the areas of highest prevalence are within Latin America (about 50–80%), parts of Eastern and Central Europe (about 20–60%), the Middle East (about 30–50%), parts of Southeast Asia (about 20–60%), and parts of Africa (about 20–55%).[26]
In the United States, data from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2004 found 9.0% of US-born persons 12–49 years of age were seropositive for IgG antibodies against T. gondii, down from 14.1% as measured in the NHANES 1988–1994.[88] In the 1999–2004 survey, 7.7% of US-born and 28.1% of foreign-born women 15–44 years of age were T. gondii seropositive.[88] A trend of decreasing seroprevalence has been observed by numerous studies in the United States and many European countries.[26] Toxoplasma gondii is considered the second leading cause of foodborne-related deaths and the fourth leading cause of foodborne-related hospitalizations in the United States.[89]
The protist responsible for toxoplasmosis is T. gondii. There are three major types of T. gondii responsible for the patterns of toxoplasmosis throughout the world. There are types I, II, and III. These three types of T. gondii have differing effects on certain hosts, mainly mice and humans due to their variation in genotypes.[90]
- Type I: virulent in mice and humans, seen in people with AIDS.
- Type II: non-virulent in mice, virulent in humans (mostly Europe and North America), seen in people with AIDS.
- Type III: non-virulent in mice, virulent mainly in animals but seen to a lesser degree in humans as well.
Current serotyping techniques can only separate type I or III from type II parasites.[91]
Because the parasite poses a particular threat to fetuses when it is contracted during pregnancy,[92] much of the global epidemiological data regarding T. gondii comes from seropositivity tests in women of childbearing age. Seropositivity tests look for the presence of antibodies against T. gondii in blood, so while seropositivity guarantees one has been exposed to the parasite, it does not necessarily guarantee one is chronically infected.[93]
History
Toxoplasma gondii was first described in 1908 by Nicolle and Manceaux in Tunisia, and independently by Splendore in Brazil.[11] Splendore reported the protozoan in a rabbit, while Nicolle and Manceaux identified it in a North African rodent, the gundi (Ctenodactylus gundi).[42] In 1909 Nicolle and Manceaux differentiated the protozoan from Leishmania.[11] Nicolle and Manceaux then named it Toxoplasma gondii after the curved shape of its infectious stage (Greek root 'toxon'= bow).[11]
The first recorded case of congenital toxoplasmosis was in 1923, but it was not identified as caused by T. gondii.[42] Janků (1923) described in detail the autopsy results of an 11-month-old boy who had presented to hospital with hydrocephalus. The boy had classic marks of toxoplasmosis including chorioretinitis (inflammation of the choroid and retina of the eye).[42] Histology revealed a number of "sporocytes", though Janků did not identify these as T. gondii.[42]
It was not until 1937 that the first detailed scientific analysis of T. gondii took place using techniques previously developed for analyzing viruses.[11] In 1937 Sabin and Olitsky analyzed T. gondii in laboratory monkeys and mice. Sabin and Olitsky showed that T. gondii was an obligate intracellular parasite and that mice fed T. gondii-contaminated tissue also contracted the infection.[11] Thus Sabin and Olitsky demonstrated T. gondii as a pathogen transmissible between animals.[citation needed]
T. gondii was first described as a human pathogen in 1939 at Babies Hospital in New York City .[11][94] Wolf, Cowen and Paige identified T. gondii infection in an infant girl delivered full-term by Caesarean section.[42] The infant developed seizures and had chorioretinitis in both eyes at three days. The infant then developed encephalomyelitis and died at one month of age. Wolf, Cowen and Paige isolated T. gondii from brain tissue lesions. Intracranial injection of brain and spinal cord samples into mice, rabbits and rats produced encephalitis in the animals.[11] Wolf, Cowen and Page reviewed additional cases and concluded that T. gondii produced recognizable symptoms and could be transmitted from mother to child.[42]
The first adult case of toxoplasmosis was reported in 1940 with no neurological signs. Pinkerton and Weinman reported the presence of Toxoplasma in a 22-year-old man from Peru who died from a subsequent bacterial infection and fever.[42]
In 1948, a serological dye test was created by Sabin and Feldman based on the ability of the patient's antibodies to alter staining of Toxoplasma.[11][95] The Sabin Feldman Dye Test is now the gold standard for identifying Toxoplasma infection.[11]
Transmission of Toxoplasma by eating raw or undercooked meat was demonstrated by Desmonts et al. in 1965 Paris.[11] Desmonts observed that the therapeutic consumption of raw beef or horse meat in a tuberculosis hospital was associated with a 50% per year increase in Toxoplasma antibodies.[11] This means that more T. gondii was being transmitted through the raw meat.
In 1974, Desmonts and Couvreur showed that infection during the first two trimesters produces most harm to the fetus, that transmission depended on when mothers were infected during pregnancy, that mothers with antibodies before pregnancy did not transmit the infection to the fetus, and that spiramycin lowered the transmission to the fetus.[42]
Toxoplasma gained more attention in the 1970s with the rise of immune-suppressant treatment given after organ or bone marrow transplants and the AIDS epidemic of the 1980s.[11] Patients with lowered immune system function are much more susceptible to disease.
Society and culture
"Crazy cat-lady"
"Crazy cat-lady syndrome" is a term coined by news organizations to describe scientific findings that link the parasite Toxoplasma gondii to several mental disorders and behavioral problems.[96][97] The suspected correlation between cat ownership in childhood and later development of schizophrenia suggested that further studies were needed to determine a risk factor for children;[98] however, later studies showed that T. gondii was not a causative factor in later psychoses.[99] Researchers also found that cat ownership does not strongly increase the risk of a T. gondii infection in pregnant women.[61][100]
The term crazy cat-lady syndrome draws on both stereotype and popular cultural reference. It was originated as instances of the aforementioned afflictions were noted amongst the populace. A cat lady is a cultural stereotype of a woman who compulsively hoards and dotes upon cats. The biologist Jaroslav Flegr is a proponent of the theory that toxoplasmosis affects human behaviour.[101][102]
Notable cases
- Tennis player Arthur Ashe developed neurological problems from toxoplasmosis (and was later found to be HIV-positive).[103]
- Actor Merritt Butrick was HIV-positive and died from toxoplasmosis as a result of his already-weakened immune system.[104]
- Pedro Zamora, reality television personality and HIV/AIDS activist, was diagnosed with toxoplasmosis as a result of his immune system being weakened by HIV.[105]
- Prince François, Count of Clermont, pretender to the throne of France had congenital toxoplasmosis; his disability caused him to be overlooked in the line of succession.
- Actress Leslie Ash contracted toxoplasmosis in the second month of pregnancy.[106]
- British middle-distance runner Sebastian Coe contracted toxoplasmosis in 1983, which was probably transmitted by a cat while he trained in Italy.[107][108]
- Tennis player Martina Navratilova experienced toxoplasmosis during the 1982 US Open.[109]
Other animals
File:Parasite140105-fig3 Toxoplasmosis in a bar-shouldered dove - TEM of 2 tachyzoites.tif File:Parasite150075-fig1 Toxoplasma gondii in Giant panda.tif
Although T. gondii has the capability of infecting virtually all warm-blooded animals, susceptibility and rates of infection vary widely between different genera and species.[112][113] Rates of infection in populations of the same species can also vary widely due to differences in location, diet, and other factors.[citation needed]
Although infection with T. gondii has been noted in several species of Asian primates, seroprevalence of T. gondii antibodies were found for the first time in toque macaques (Macaca sinica) that are endemic to the island of Sri Lanka.[114]
Australian marsupials are particularly susceptible to toxoplasmosis.[115] Wallabies, koalas, wombats, pademelons and small dasyurids can be killed by it, with eastern barred bandicoots typically dying within about 3 weeks of infection.[116]
It is estimated that 23% of wild swine worldwide are seropositive for T. gondii.[117] Seroprevalence varies across the globe with the highest seroprevalence in North America (32%) and Europe (26%) and the lowest in Asia (13%) and South America (5%).[117] Geographical regions located at higher latitudes and regions that experience warmer, humid climates are associated with increased seroprevalence of T. gondii among wild boar.[117] Wild boar infected with T. gondii pose a potential health risk for humans who consume their meat.[117]
Livestock
Among livestock, pigs,[118][119][120] sheep[121] and goats have the highest rates of chronic T. gondii infection.[122] The prevalence of T. gondii in meat-producing animals varies widely both within and among countries,[122] and rates of infection have been shown to be dramatically influenced by varying farming and management practices.[14] For instance, animals kept outdoors or in free-ranging environments are more at risk of infection than animals raised indoors or in commercial confinement operations.[14][47]
Pigs
Worldwide, the percentage of pigs harboring viable parasites has been measured to be 3–71.43%[120] and in the United States (via bioassay in mice or cats) to be as high as 92.7% and as low as 0%, depending on the farm or herd.[47] Surveys of seroprevalence (T. gondii antibodies in blood) are more common, and such measurements are indicative of the high relative seroprevalence in pigs across the world.[123] Neonatal piglets have been found to experience the entire range of severity, including progression to stillbirth.[124][118]:95 This was especially demonstrated in the foundational Thiptara et al. 2006, reporting a litter birth of three stillborns and six live in Thailand. This observation has been relevant not only to that country but to toxoplasmosis control in porciculture around the world.[125][118]:95[120]
Sheep
Along with pigs, sheep and goats are among the most commonly infected livestock of epidemiological significance for human infection.[122] Prevalence of viable T. gondii in sheep tissue has been measured (via bioassay) to be as high as 78% in the United States,[126] and a 2011 survey of goats intended for consumption in the United States found a seroprevalence of 53.4%.[127]
Chickens
Due to a lack of exposure to the outdoors, chickens raised in large-scale indoor confinement operations are not commonly infected with T. gondii.[14] Free-ranging or backyard-raised chickens are much more commonly infected.[14] A survey of free-ranging chickens in the United States found its prevalence to be 17–100%, depending on the farm.[128] Because chicken meat is generally cooked thoroughly before consumption, poultry is not generally considered to be a significant risk factor for human T. gondii infection.[129]
Cattle
Although cattle and buffalo can be infected with T. gondii, the parasite is generally eliminated or reduced to undetectable levels within a few weeks following exposure.[14] Tissue cysts are rarely present in buffalo meat or beef, and meat from these animals is considered to be low-risk for harboring viable parasites.[47][122][130]
Horses
Horses are considered resistant to chronic T. gondii infection.[14] However, viable cells have been isolated from US horses slaughtered for export, and severe human toxoplasmosis in France has been epidemiologically linked to the consumption of horse meat.[47][131]
Domestic cats
In 1942, the first case of feline toxoplasmosis was diagnosed and reported in a domestic cat in Middletown, New York.[132] The investigators isolated oocysts from feline feces and found that the oocysts could be infectious for up to 12 months in the environment.[133]
The seroprevalence of T. gondii in domestic cats, worldwide has been estimated to be around 30–40%[134] and exhibits significant geographical variation. In the United States, no official national estimate has been made, but local surveys have shown levels varying between 16% and 80%.[134] A 2012 survey of 445 purebred pet cats and 45 shelter cats in Finland found an overall seroprevalence of 48.4%,[135] while a 2010 survey of feral cats from Giza, Egypt found a seroprevalence rate of 97.4%.[136] Another survey from Colombia recorded seroprevalence of 89.3%,[137] whereas a Chinese (Guangdong) study found just a 2.1% prevalence.[138]
T. gondii infection rates in domestic cats vary widely depending on the cats' diets and lifestyles.[139] Feral cats that hunt for their food are more likely to be infected than domestic cats, and naturally also depends on the prevalence of T. gondii-infected prey such as birds and small mammals.[140]
Most infected cats will shed oocysts only once in their lifetimes, for a period of about one to two weeks.[134] This shedding can release millions of oocysts, each capable of spreading and surviving for months.[134] An estimated 1% of cats at any given time are actively shedding oocysts.[14]
It is difficult to control the cat population with the infected oocysts due to lack of an effective vaccine. This remains a challenge in most cases and the programs that are readily available are questionable in efficacy.[141]
Rodents
Infection with T. gondii has been shown to alter the behavior of mice and rats in ways thought to increase the rodents' chances of being preyed upon by cats.[142][143][144] Infected rodents show a reduction in their innate aversion to cat odors; while uninfected mice and rats will generally avoid areas marked with cat urine or with cat body odor, this avoidance is reduced or eliminated in infected animals.[142][144][145] Moreover, some evidence suggests this loss of aversion may be specific to feline odors: when given a choice between two predator odors (cat or mink), infected rodents show a significantly stronger preference to cat odors than do uninfected controls.[146][147]
In rodents, T. gondii–induced behavioral changes occur through epigenetic remodeling in neurons associated with observed behaviors;[148][149] for example, it modifies epigenetic methylation to induce hypomethylation of arginine vasopressin-related genes in the medial amygdala to greatly decrease predator aversion.[148][149] Similar epigenetically induced behavioral changes have also been observed in mouse models of addiction, where changes in the expression of histone-modifying enzymes via gene knockout or enzyme inhibition in specific neurons produced alterations in drug-related behaviors.[150][151][152] Widespread histone–lysine acetylation in cortical astrocytes appears to be another epigenetic mechanism employed by T. gondii.[153][154]
T. gondii-infected rodents show a number of behavioral changes beyond altered responses to cat odors. Rats infected with the parasite show increased levels of activity and decreased neophobic behavior.[155] Similarly, infected mice show alterations in patterns of locomotion and exploratory behavior during experimental tests. These patterns include traveling greater distances, moving at higher speeds, accelerating for longer periods of time, and showing a decreased pause-time when placed in new arenas.[156] Infected rodents have also been shown to have lower anxiety, using traditional models such as elevated plus mazes, open field arenas, and social interaction tests.[156][157]
Marine mammals
A University of California, Davis study of dead sea otters collected from 1998 to 2004 found toxoplasmosis was the cause of death for 13% of the animals.[158] Proximity to freshwater outflows into the ocean was a major risk factor. Ingestion of oocysts from cat feces is considered to be the most likely ultimate source.[159] Surface runoff containing wild cat feces and litter from domestic cats flushed down toilets are possible sources of oocysts.[160][161] These same sources may have also introduced the toxoplasmosis infection to the endangered Hawaiian monk seal.[162] Infection with the parasite has contributed to the death of at least four Hawaiian monk seals.[162] A Hawaiian monk seal's infection with T. gondii was first noted in 2004.[163] The parasite's spread threatens the recovery of this highly endangered pinniped. The parasites have been found in dolphins and whales.[164][165] Researchers Black and Massie believe anchovies, which travel from estuaries into the open ocean, may be helping to spread the disease.[166]
Giant panda
Toxoplasma gondii has been reported as the cause of death of a giant panda kept in a zoo in China, who died in 2014 of acute gastroenteritis and respiratory disease.[111] Although seemingly anecdotal, this report emphasizes that all warm-blooded species are likely to be infected by T. gondii, including endangered species such as the giant panda.[citation needed]
Research
Chronic infection with T. gondii has traditionally been considered asymptomatic in people with normal immune function.[167] Some evidence suggests latent infection may subtly influence a range of human behaviors and tendencies, and infection may alter the susceptibility to or intensity of a number of psychiatric or neurological disorders.[168][167]
In most of the current studies where positive correlations have been found between T. gondii antibody titers and certain behavioral traits or neurological disorders, T. gondii seropositivity tests are conducted after the onset of the examined disease or behavioral trait; that is, it is often unclear whether infection with the parasite increases the chances of having a certain trait or disorder, or if having a certain trait or disorder increases the chances of becoming infected with the parasite.[169] Groups of individuals with certain behavioral traits or neurological disorders may share certain behavioral tendencies that increase the likelihood of exposure to and infection with T. gondii; as a result, it is difficult to confirm causal relationships between T. gondii infections and associated neurological disorders or behavioral traits.[169]
Mental health
Some evidence links T. gondii to schizophrenia.[167] Two 2012 meta-analyses found that the rates of antibodies to T. gondii in people with schizophrenia were 2.7 times higher than in controls.[170][171] T. gondii antibody positivity was therefore considered an intermediate risk factor in relation to other known risk factors.[170] Cautions noted include that the antibody tests do not detect toxoplasmosis directly, most people with schizophrenia do not have antibodies for toxoplasmosis, and publication bias might exist.[171] While the majority of these studies tested people already diagnosed with schizophrenia for T. gondii antibodies, associations between T. gondii and schizophrenia have been found prior to the onset of schizophrenia symptoms.[142] Sex differences in the age of schizophrenia onset may be explained in part by a second peak of T. gondii infection incidence during ages 25–30 in females only.[172] Although a mechanism supporting the association between schizophrenia and T. gondii infection is unclear, studies have investigated a molecular basis of this correlation.[172] Antipsychotic drugs used in schizophrenia appear to inhibit the replication of T. gondii tachyzoites in cell culture.[142] Supposing a causal link exists between T. gondii and schizophrenia, studies have yet to determine why only some individuals with latent toxoplasmosis develop schizophrenia; some plausible explanations include differing genetic susceptibility, parasite strain differences, and differences in the route of the acquired T. gondii infection.[173]
Correlations have also been found between antibody titers to T. gondii and OCD, as well as suicide among people with mood disorders including bipolar disorder.[168][174] Positive antibody titers to T. gondii appear to be uncorrelated with major depression or dysthymia.[175] Although there is a correlation between T. gondii and many psychological disorders, the underlying mechanism is unclear. A 2016 study of 236 persons with high levels of toxoplasmosis antibodies found that "there was little evidence that T. gondii was related to increased risk of psychiatric disorder, poor impulse control, personality aberrations or neurocognitive impairment".[176]
Neurological disorders
Latent infection has been linked to Parkinson's disease and Alzheimer's disease.[168]
Individuals with multiple sclerosis show infection rates around 15% lower than the general public.[177]
Traffic accidents
Latent T. gondii infection in humans has been associated with a higher risk of automobile accidents,[178] potentially due to impaired psychomotor performance or enhanced risk-taking personality profiles.[168]
Climate change
Climate change has been reported to affect the occurrence, survival, distribution and transmission of T. gondii.[179] T. gondii has been identified in the Canadian arctic, a location that was once too cold for its survival.[180] Higher temperatures increase the survival time of T. gondii.[179] More snowmelt and precipitation can increase the amount of T. gondii oocysts that are transported via river flow.[179] Shifts in bird, rodent, and insect populations and migration patterns can impact the distribution of T. gondii due to their role as reservoir and vector.[179] Urbanization and natural environmental degradation are also suggested to affect T. gondii transmission and increase risk of infection.[179]
See also
- Toxoplasmic chorioretinitis
- TORCH infection
- Pyrimethamine
References
- ↑ 1.0 1.1 1.2 1.3 1.4 "Parasites – Toxoplasmosis (Toxoplasma infection) Disease". July 10, 2014. https://www.cdc.gov/parasites/toxoplasmosis/disease.html.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Hunter, CA; Sibley, LD (November 2012). "Modulation of innate immunity by Toxoplasma gondii virulence effectors". Nature Reviews Microbiology 10 (11): 766–78. doi:10.1038/nrmicro2858. PMID 23070557.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 "Parasites – Toxoplasmosis (Toxoplasma infection) Epidemiology & Risk Factors". March 26, 2015. https://www.cdc.gov/parasites/toxoplasmosis/epi.html.
- ↑ 4.0 4.1 "Parasites – Toxoplasmosis (Toxoplasma infection) Diagnosis". January 10, 2013. https://www.cdc.gov/parasites/toxoplasmosis/diagnosis.html.
- ↑ 5.0 5.1 5.2 "Parasites – Toxoplasmosis (Toxoplasma infection) Resources for Health Professionals". April 14, 2014. https://www.cdc.gov/parasites/toxoplasmosis/health_professionals/index.html#tx.
- ↑ 6.0 6.1 6.2 6.3 Torgerson, Paul R; Mastroiacovo, Pierpaolo (2013). "The global burden of congenital toxoplasmosis: a systematic review". Bulletin of the World Health Organization 91 (7): 501–508. doi:10.2471/BLT.12.111732. ISSN 0042-9686. PMID 23825877.
- ↑ 7.0 7.1 7.2 7.3 7.4 "Toxoplasmosis—a global threat. Correlation of latent toxoplasmosis with specific disease burden in a set of 88 countries". PLOS ONE 9 (3): e90203. March 2014. doi:10.1371/journal.pone.0090203. PMID 24662942. Bibcode: 2014PLoSO...990203F. "Toxoplasmosis is becoming a global health hazard as it infects 30–50% of the world human population.".
- ↑ "Toxoplasma gondii: An Underestimated Threat?". Trends in Parasitology 36 (12): 959–969. December 2020. doi:10.1016/j.pt.2020.08.005. PMID 33012669. "Accumulating evidence suggests that latent infection of Toxoplasma gondii is associated with a variety of neuropsychiatric and behavioral conditions.".
- ↑ 9.0 9.1 "Parasites – Toxoplasmosis (Toxoplasma infection) Biology". March 17, 2015. https://www.cdc.gov/parasites/toxoplasmosis/biology.html.
- ↑ 10.0 10.1 "Parasites – Toxoplasmosis (Toxoplasma infection) Prevention & Control". January 10, 2013. https://www.cdc.gov/parasites/toxoplasmosis/prevent.html.
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 11.12 11.13 Ferguson DJ (2009). "Toxoplasma gondii: 1908–2008, homage to Nicolle, Manceaux and Splendore". Memórias do Instituto Oswaldo Cruz 104 (2): 133–48. doi:10.1590/S0074-02762009000200003. PMID 19430635.
- ↑ Tyebji, S; Seizova, S; Hannan, AJ; Tonkin, CJ (January 2019). "Toxoplasmosis: A pathway to neuropsychiatric disorders.". Neuroscience and Biobehavioral Reviews 96: 72–92. doi:10.1016/j.neubiorev.2018.11.012. PMID 30476506.
- ↑ 13.0 13.1 "Immune response and immunopathology during toxoplasmosis". Seminars in Immunopathology 34 (6): 793–813. 2012. doi:10.1007/s00281-012-0339-3. PMID 22955326.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 14.6 14.7 14.8 "Toxoplasma gondii infection in humans and animals in the United States". International Journal for Parasitology 38 (11): 1257–78. September 2008. doi:10.1016/j.ijpara.2008.03.007. PMID 18508057.
- ↑ 15.0 15.1 "toxoplasmosis". http://www.mayoclinic.org/diseases-conditions/toxoplasmosis/basics/symptoms/con-20025859.
- ↑ "Toxoplasma gondii infection in the United States: seroprevalence and risk factors". American Journal of Epidemiology 154 (4): 357–65. 2001. doi:10.1093/aje/154.4.357. PMID 11495859.
- ↑ "Tachyzoite – an overview | ScienceDirect Topics". https://www.sciencedirect.com/topics/immunology-and-microbiology/tachyzoite#:~:text=Tachyzoites%20are%20found%20in%20all,lymph%20nodes,%20and%20the%20CNS..
- ↑ Paul M (1 July 1999). "Immunoglobulin G Avidity in Diagnosis of Toxoplasmic Lymphadenopathy and Ocular Toxoplasmosis". Clin. Diagn. Lab. Immunol. 6 (4): 514–8. doi:10.1128/CDLI.6.4.514-518.1999. PMID 10391853.
- ↑ "Lymphadenopathy". UK Neqas Micro. http://ukneqasmicro.org.uk/parasitology/images/pdf/ToxoplasmaSerology/Immunocompetent/Lymphadenopathy.pdf.
- ↑ "CDC Parasites – Toxoplasmosis (Toxoplasma infection) – Disease". https://www.cdc.gov/parasites/toxoplasmosis/disease.html.
- ↑ "Acute fatal toxoplasmosis in squirrels (Sciurus carolensis) with bradyzoites in visceral tissues". The Journal of Parasitology 92 (3): 658–9. 2006. doi:10.1645/GE-749R.1. PMID 16884019.
- ↑ Nawaz Khan, A (2015). "Imaging in CNS Toxoplasmosis". Medscape Web Site. http://emedicine.medscape.com/article/344706-overview..
- ↑ 23.0 23.1 "Persistence of Toxoplasma gondii in the central nervous system: a fine-tuned balance between the parasite, the brain and the immune system". Parasite Immunology 37 (3): 150–158. 2015. doi:10.1111/pim.12173. PMID 25573476. "The seroprevalence of T. gondii in humans varies between 10 and 70% worldwide, depending on the region and increases significantly with age. Upon infection, the parasites persist as intraneuronal cysts in the central nervous system (CNS) for the lifetime of the host (1, Figure 1). Until recently, parasite persistence in healthy individuals was regarded as clinically asymptomatic. However, in the last decade, several reports have indicated that chronic cerebral toxoplasmosis may impact on the behaviour of its host (2).".
- ↑ Randall Parker: Humans Get Personality Altering Infections From Cats . September 30, 2003
- ↑ 25.0 25.1 "Toxoplasma gondii-induced neuronal alterations". Parasite Immunology 37 (3): 159–170. March 2015. doi:10.1111/pim.12157. PMID 25376390. "The zoonotic pathogen Toxoplasma gondii infects over 30% of the human population. The intracellular parasite can persist lifelong in the CNS within neurons modifying their function and structure, thus leading to specific behavioural changes of the host. ... Furthermore, investigations of the human population have correlated Toxoplasma seropositivity with changes in neurological functions; however, the complex underlying mechanisms of the subtle behavioural alteration are still not fully understood. The parasites are able to induce direct modifications in the infected cells, for example by altering dopamine metabolism, by functionally silencing neurons as well as by hindering apoptosis.".
- ↑ 26.0 26.1 26.2 26.3 "Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis". International Journal for Parasitology 39 (12): 1385–94. October 2009. doi:10.1016/j.ijpara.2009.04.003. PMID 19433092.
- ↑ ""Latent" infection with Toxoplasma gondii: association with trait aggression and impulsivity in healthy adults". Journal of Psychiatric Research 60: 87–94. 2015. doi:10.1016/j.jpsychires.2014.09.019. PMID 25306262.
- ↑ "Latent Toxoplasmosis gondii: emerging evidence for influences on neuropsychiatric disorders". Journal of Neuropsychiatry and Clinical Neurosciences 24 (4): 376–83. 2012. doi:10.1176/appi.neuropsych.12100234. PMID 23224444. "Nine of eleven studies using the Cattell's 16-Personality Factor self-report questionnaire found significant and consistent results for both genders. Seropositive men overall had lower regard for rules and higher vigilance (suspicious, jealous, rigid/inflexible) than seronegative men. In contrast, seropositive women had greater regard for rules and higher warmth than seronegative women. Both seropositive genders were more anxious than matched healthy-comparison subjects. ... Behavioral observations and interviews were completed to ascertain whether the gender differences found in self-report measures were replicated by objective measures. Seropositive men scored significantly lower than seronegative men on Self-Control, Clothes Tidiness, and Relationships. The differences were less impressive for the seropositive women, with only trends toward higher scores on Self-Control and Clothes Tidiness as compared with seronegative women. The authors view the study results as objective confirmation that T. gondii presence can change a human host's behaviors.".
- ↑ Gohardehi, S; Sharif, M; Sarvi, S; Moosazadeh, M; Alizadeh-Navaei, R; Hosseini, SA; Amouei, A; Pagheh, A et al. (August 2018). "The potential risk of toxoplasmosis for traffic accidents: A systematic review and meta-analysis.". Experimental Parasitology 191: 19–24. doi:10.1016/j.exppara.2018.06.003. PMID 29906469.
- ↑ Zimmermann, Stefan; Hadaschik, Eva; Dalpke, Alexander; Hassel, Jessica C.; Ajzenberg, Daniel; Tenner-Racz, Klara; Lehners, Nicola; Kapaun, Annette et al. (2013-04-01). "Varicella-Like Cutaneous Toxoplasmosis in a Patient with Aplastic Anemia" (in en). Journal of Clinical Microbiology 51 (4): 1341–1344. doi:10.1128/JCM.02851-12. ISSN 0095-1137. PMID 23390283.
- ↑ Template:Fitzpatrick 6
- ↑ 32.0 32.1 32.2 Robert-Gangneux, F.; Darde, M.-L. (2012). "Epidemiology of and Diagnostic Strategies for Toxoplasmosis". Clinical Microbiology Reviews 25 (2): 264–296. doi:10.1128/CMR.05013-11. ISSN 0893-8512. PMID 22491772.
- ↑ Markus, MB (1987). "Terms for coccidian merozoites". Annals of Tropical Medicine and Parasitology 81 (4): 463. doi:10.1080/00034983.1987.11812147. PMID 3446034.
- ↑ 34.0 34.1 34.2 34.3 34.4 Miller CM; Boulter NR; Ikin RJ; Smith NC (January 2009). "The immunobiology of the innate response to Toxoplasma gondii". International Journal for Parasitology 39 (1): 23–39. doi:10.1016/j.ijpara.2008.08.002. PMID 18775432.
- ↑ Brasil, Thaís Rigueti; Freire-de-Lima, Celio Geraldo; Morrot, Alexandre; Vetö Arnholdt, Andrea Cristina (2017). "Host-Toxoplasma gondii Coadaptation Leads to Fine Tuning of the Immune Response". Frontiers in Immunology 8: 1080. doi:10.3389/fimmu.2017.01080. PMID 28955329.
- ↑ 36.0 36.1 36.2 Martens S; Parvanova I; Zerrahn J; Griffiths G; Schell G; Reichmann G; Howard JC (November 2005). "Disruption of Toxoplasma gondii parasitophorous vacuoles by the mouse p47-resistance GTPases". PLOS Pathogens 1 (3): e24. doi:10.1371/journal.ppat.0010024. PMID 16304607.
- ↑ 37.0 37.1 Denkers, EY; Schneider, AG; Cohen, AB; Butcher, BA (2012). "Phagocyte responses to protozoan infection and how Toxoplasma gondii meets the challenge". PLOS Pathogens 8 (8): e1002794. doi:10.1371/journal.ppat.1002794. PMID 22876173.
- ↑ 38.0 38.1 38.2 "Toxoplasma gondii infection confers resistance against BimS-induced apoptosis by preventing the activation and mitochondrial targeting of pro-apoptotic Bax". Journal of Cell Science 122 (Pt 19): 3511–21. 2009. doi:10.1242/jcs.050963. PMID 19737817.
- ↑ 39.0 39.1 39.2 "Host cell autophagy is induced by Toxoplasma gondii and contributes to parasite growth". The Journal of Biological Chemistry 284 (3): 1694–701. 2009. doi:10.1074/jbc.M807890200. PMID 19028680.
- ↑ 40.0 40.1 "Host cell manipulation by the human pathogen Toxoplasma gondii". Cellular and Molecular Life Sciences 65 (12): 1900–15. 2008. doi:10.1007/s00018-008-7556-x. PMID 18327664.
- ↑ Hoeve, Arne L. ten; Braun, Laurence; Rodriguez, Matias E.; Olivera, Gabriela C.; Bougdour, Alexandre; Belmudes, Lucid; Couté, Yohann; Saeij, Jeroen P. J. et al. (2022-11-09). "The Toxoplasma effector GRA28 promotes parasite dissemination by inducing dendritic cell-like migratory properties in infected macrophages" (in English). Cell Host & Microbe 30 (11): 1570–1588.e7. doi:10.1016/j.chom.2022.10.001. ISSN 1931-3128. PMID 36309013.
- ↑ 42.0 42.1 42.2 42.3 42.4 42.5 42.6 42.7 42.8 "Toxoplasmosis: A history of clinical observations". International Journal for Parasitology 39 (8): 895–901. 2009. doi:10.1016/j.ijpara.2009.02.004. PMID 19217908.
- ↑ Toxoplasma gondii: the model apicomplexan: perspectives and methods. Elsevier/Academic Press. 2007. ISBN 9780123695420. https://archive.org/details/toxoplasmagondii0000unse.
- ↑ 44.0 44.1 44.2 Derouin, F; Pelloux, H; ESCMID Study Group on Clinical, Parasitology. (December 2008). "Prevention of toxoplasmosis in transplant patients". Clinical Microbiology and Infection 14 (12): 1089–101. doi:10.1111/j.1469-0691.2008.02091.x. PMID 19018809.
- ↑ 45.0 45.1 Khurana, Sumeeta; Batra, Nitya (2016). "Toxoplasmosis in organ transplant recipients: Evaluation, implication, and prevention". Tropical Parasitology 6 (2): 123–128. doi:10.4103/2229-5070.190814. PMID 27722100.
- ↑ "Toxoplasmosis". Centers of Disease Control and Prevention. 2004-11-22. http://www.dpd.cdc.gov/DPDx/HTML/Toxoplasmosis.htm.
- ↑ 47.0 47.1 47.2 47.3 47.4 "Foodborne toxoplasmosis". Clinical Infectious Diseases 55 (6): 845–51. September 2012. doi:10.1093/cid/cis508. PMID 22618566.
- ↑ Dubey, J.P.. "Swine Toxoplasmosis". http://www.ncagr.gov/vet/FactSheets/Toxoplasmosis.htm.
- ↑ Signori Pereira, Karen; Franco, Regina; Leal, Diego (2010). "Transmission of Toxoplasmosis (Toxoplasma gondii) by Foods". Advances in Food Nutrition and Research. Advances in Food and Nutrition Research 60: 1–19. doi:10.1016/S1043-4526(10)60001-0. ISBN 9780123809445. PMID 20691951.
- ↑ Boughattas, Sonia (2 September 2017). "Toxoplasma infection and milk consumption: Meta-analysis of assumptions and evidences". Crit Rev Food Sci Nutr. 57 (13): 2924–2933. doi:10.1080/10408398.2015.1084993. PMID 26467987. https://pubmed.ncbi.nlm.nih.gov/26467987/. Retrieved 8 November 2023.
- ↑ Jones, Jeffrey; Dargelas, Valerie; Roberts, Jacquelin; Press, Cindy; Remington, Jack; Montoya, Jose (15 September 2009). "Risk Factors for Toxoplasma gondii Infection in the United States". Clinical Infectious Diseases 49 (6): 878–884. doi:10.1086/605433. PMID 19663709.
- ↑ "Parasites – Toxoplasmosis (Toxoplasma infection)". Centers of Disease Control and Prevention. 2011-04-05. https://www.cdc.gov/parasites/toxoplasmosis/biology.html.
- ↑ Assadi-Rad, A.M.; New, John C.; Patton, Sharon (April 1995). "Risk factors associated with transmission of Toxoplasma gondii to sows kept in different management systems in Tennessee". Veterinary Parasitology 57 (4): 289–297. doi:10.1016/0304-4017(94)00677-5. PMID 7660566.
- ↑ 54.0 54.1 Coster, LO (June 2013). "Parasitic infections in solid organ transplant recipients". Infectious Disease Clinics of North America 27 (2): 395–427. doi:10.1016/j.idc.2013.02.008. PMID 23714347.
- ↑ 55.0 55.1 "Diagnosis of congenital toxoplasmosis by polymerase chain reaction on neonatal peripheral blood". Diagnostic Microbiology and Infectious Disease 71 (2): 174–6. 2011. doi:10.1016/j.diagmicrobio.2011.06.006. PMID 21856107.
- ↑ 56.0 56.1 56.2 Di Mario, S; Basevi, V; Gagliotti, C; Spettoli, D; Gori, G; D'Amico, R; Magrini, N (23 October 2015). "Prenatal education for congenital toxoplasmosis". Cochrane Database of Systematic Reviews 2015 (10): CD006171. doi:10.1002/14651858.CD006171.pub4. PMID 26493047. PMC 9272404. https://iris.unimore.it/bitstream/11380/1082489/2/Mario_et_al-2015-The_Cochrane_Library.sup-2.pdf.
- ↑ "Circular Normativa sobre Cuidados Pré-Concepcionais – Direcção-Geral de Saúde". http://www.srsdocs.com/parcerias/normas/circulares/dgs/2006/cuidados_pre_concepcionais.pdf.
- ↑ 58.0 58.1 58.2 58.3 Sukthana Y (March 2006). "Toxoplasmosis: beyond animals to humans". Trends in Parasitology 22 (3): 137–42. doi:10.1016/j.pt.2006.01.007. PMID 16446116.
- ↑ [1]
- ↑ 60.0 60.1 "Seroprevalence and incidence of Toxoplasma gondii infection in the Legnano area of Italy". Clinical Microbiology and Infection 14 (2): 186–9. 2008. doi:10.1111/j.1469-0691.2007.01883.x. PMID 18034857.
- ↑ 61.0 61.1 61.2 61.3 61.4 Kapperud, Georg; Jenum, Pal A.; Stray-Pedersen, Babill; Melby, Kjetil K.; Eskild, Anne; Eng, Jan (1996). "Risk factors for Toxoplasma gondii infection in pregnancy. Results of a prospective case-control study in Norway". American Journal of Epidemiology 144 (4): 405–412. doi:10.1093/oxfordjournals.aje.a008942. PMID 8712198.
- ↑ 62.0 62.1 62.2 62.3 "Toxoplasma gondii: transmission, diagnosis and prevention". Clinical Microbiology and Infection 8 (10): 634–40. 2002. doi:10.1046/j.1469-0691.2002.00485.x. PMID 12390281.
- ↑ "Sources of toxoplasma infection in pregnant women: European multicentre case-control study. European Research Network on Congenital Toxoplasmosis". BMJ 321 (7254): 142–7. Jul 15, 2000. doi:10.1136/bmj.321.7254.142. PMID 10894691.
- ↑ "Risk factors for Toxoplasma infection in a reproductive age female population in the area of Belgrade, Yugoslavia". European Journal of Epidemiology 14 (6): 605–10. September 1998. doi:10.1023/A:1007461225944. PMID 9794128.
- ↑ "Risk Factors forToxoplasma gondiiInfection in the United States". Clinical Infectious Diseases 49 (6): 878–884. 2009. doi:10.1086/605433. PMID 19663709.
- ↑ "Women infected with parasite Toxoplasma have more sons". Die Naturwissenschaften 94 (2): 122–7. 2007. doi:10.1007/s00114-006-0166-2. PMID 17028886. Bibcode: 2007NW.....94..122K.
- ↑ Ian Sample, science correspondent (2006-10-12). "Pregnant women infected by cat parasite more likely to give birth to boys, say researchers | Science". The Guardian (London). https://www.theguardian.com/science/2006/oct/12/uk.health.
- ↑ "Recent trends in molecular diagnostics for Toxoplasma gondii infections". Clinical Microbiology and Infection 11 (3): 170–6. 2005. doi:10.1111/j.1469-0691.2004.01073.x. PMID 15715713.
- ↑ 69.0 69.1 69.2 69.3 Montoya JG (2002). "Laboratory diagnosis of Toxoplasma gondii infection and toxoplasmosis". The Journal of Infectious Diseases 185 (Suppl 1): S73–82. doi:10.1086/338827. PMID 11865443.
- ↑ 70.0 70.1 70.2 "Neglected parasitic infections in the United States: toxoplasmosis". American Journal of Tropical Medicine and Hygiene 90 (5): 794–9. 2014. doi:10.4269/ajtmh.13-0722. PMID 24808246.
- ↑ Remington, J. S.; Thulliez, P.; Montoya, J. G. (2004). "Recent Developments for Diagnosis of Toxoplasmosis". Journal of Clinical Microbiology 42 (3): 941–945. doi:10.1128/JCM.42.3.941-945.2004. ISSN 0095-1137. PMID 15004036.
- ↑ 72.0 72.1 Robert-Gangneux, Florence; Guegan, Hélène (2021). "Anti-Toxoplasma IgG assays: What performances for what purpose? A systematic review". Parasite 28: 39. doi:10.1051/parasite/2021035. PMID 33904818.

- ↑ Sensini, A. (2006). "Toxoplasma gondii infection in pregnancy: opportunities and pitfalls of serological diagnosis". Clinical Microbiology and Infection 12 (6): 504–512. doi:10.1111/j.1469-0691.2006.01444.x. ISSN 1198-743X. PMID 16700697.
- ↑ 74.0 74.1 74.2 74.3 74.4 74.5 "Real-time PCR for quantitative detection of Toxoplasma gondii". Journal of Clinical Microbiology 38 (11): 4121–5. 2000. doi:10.1128/JCM.38.11.4121-4125.2000. PMID 11060078.
- ↑ Jones, J; Lopez, A; Wilson, M (15 May 2003). "Congenital toxoplasmosis". American Family Physician 67 (10): 2131–8. PMID 12776962.
- ↑ "Congenital toxoplasmosis: MedlinePlus Medical Encyclopedia" (in en). https://medlineplus.gov/ency/article/001360.htm.
- ↑ Corrêa, Camila de Castro; Maximino, Luciana Paula; Weber, Silke Anna Theresa (July 2018). "Hearing Disorders in Congenital Toxoplasmosis: A Literature Review". International Archives of Otorhinolaryngology 22 (3): 330–333. doi:10.1055/s-0037-1605377. ISSN 1809-9777. PMID 29983776.
- ↑ Macedo de Resende, Luciana. "Congenital toxoplasmosis: Auditory and language outcomes in early diagnosed and treated children". http://revistaseletronicas.pucrs.br/ojs/index.php/scientiamedica/article/viewFile/5927/5053.
- ↑ "Endochin-like quinolones are highly efficacious against acute and latent experimental toxoplasmosis". Proceedings of the National Academy of Sciences of the United States of America 109 (39): 15936–41. 2012. doi:10.1073/pnas.1208069109. PMID 23019377. Bibcode: 2012PNAS..10915936D.
- ↑ "Role of clindamycin in the treatment of central nervous system toxoplasmosis". American Journal of Medicine 83 (3): 551–554. 1987. doi:10.1016/0002-9343(87)90769-8. PMID 3661590.
- ↑ "CDC – Toxoplasmosis – Resources for Health Professionals". https://www.cdc.gov/parasites/toxoplasmosis/health_professionals/index.html#tx.
- ↑ "Toxoplasmosis – treatment key research". NAM & aidsmap. 2005-11-02. http://www.aidsmap.com/cms1032641.asp.
- ↑ "Efficacy of atovaquone combined with clindamycin against murine infection with a cystogenic (Me49) strain of Toxoplasma gondii". Journal of Antimicrobial Chemotherapy 50 (6): 981–7. 2002. doi:10.1093/jac/dkf251. PMID 12461021.
- ↑ "Congenital toxoplasmosis". American Family Physician 67 (10): 2131–8. 2003. PMID 12776962.
- ↑ "Why prevent, diagnose and treat congenital toxoplasmosis?". Memórias do Instituto Oswaldo Cruz 104 (2): 320–44. 2009. doi:10.1590/s0074-02762009000200029. PMID 19430661.
- ↑ "Outcome of Treatment for Congenital Toxoplasmosis, 1981–2004: The National Collaborative Chicago-Based, Congenital Toxoplasmosis Study". Clinical Infectious Diseases 42 (10): 1383–1394. 15 May 2006. doi:10.1086/501360. PMID 16619149.
- ↑ "Congenital Toxoplasmosis". https://www.babysfirsttest.org/newborn-screening/conditions/congenital-toxoplasmosis.
- ↑ 88.0 88.1 "Toxoplasma gondii infection in the United States, 1999 2004, decline from the prior decade". American Journal of Tropical Medicine and Hygiene 77 (3): 405–10. September 2007. doi:10.4269/ajtmh.2007.77.405. PMID 17827351.
- ↑ Scallan, Elaine; Hoekstra, Robert; Angulo, Frederick; Tauxe, Robert; Widdowson, Marc-Alain; Roy, Sharon; Jones, Jeffery; Griffin, Patricia (January 2011). "Foodborne Illness Acquired in the United States - Major Pathogens". Emerging Infectious Diseases 17 (1): 7–15. doi:10.3201/eid1701.P11101. PMID 21192848.
- ↑ "Latent Toxoplasmosis and Human". Iranian Journal of Parasitology 7 (1): 1–17. 2011. PMID 23133466. PMC 3488815. http://ijpa.tums.ac.ir/index.php/ijpa/article/view/214.
- ↑ Sibley LD; Khan A; Ajioka JW; Rosenthal BM (2009). "Genetic diversity of Toxoplasma gondii in animals and humans". Philosophical Transactions of the Royal Society B: Biological Sciences 364 (1530): 2749–2761. doi:10.1098/rstb.2009.0087. PMID 19687043.
- ↑ "CDC: Parasites – Toxoplasmosis (Toxoplasma infection) – Pregnant Women". https://www.cdc.gov/parasites/toxoplasmosis/gen_info/pregnant.html.
- ↑ "Toxoplasmosis of rats: a review, with considerations of their value as an animal model and their possible role in epidemiology". Veterinary Parasitology 77 (1): 1–32. May 1998. doi:10.1016/S0304-4017(97)00227-6. PMID 9652380. https://zenodo.org/record/1260015.
- ↑ Tucker, Abigail (2016). The Lion In the Living Room: How House Cats Tamed Us And Took Over the World. Simon & Schuster. p. 108. ISBN 978-1-4767-3823-9.
- ↑ "Laboratory Tests For The Diagnosis Of Toxoplasmosis". Toxoplasma Serology Laboratory. http://www.pamf.org/serology/clinicianguide.html#toxosero.
- ↑ "How Your Cat Is Making You Crazy – Kathleen McAuliffe". The Atlantic. 2012-02-06. https://www.theatlantic.com/magazine/archive/2012/03/how-your-cat-is-making-you-crazy/308873/. Retrieved 2013-06-03.
- ↑ "'Cat Lady' Conundrum – Rebecca Skloot". The New York Times. 2007-12-09. https://www.nytimes.com/2007/12/09/magazine/09_10_catcoat.html.
- ↑ Torrey, E.; Simmons, Wendy; Yolken, Robert (June 2015). "Is childhood cat ownership a risk factor for schizophrenia later in life?". Schizophrenia Research 165 (1): 1–2. doi:10.1016/j.schres.2015.03.036. PMID 25892720.
- ↑ Solmi, F.; Hayes, J. F.; Lewis, G.; Kirkbride, J. B. (July 31, 2017). "Curiosity killed the cat: no evidence of an association between cat ownership and psychotic symptoms at ages 13 and 18 years in a UK general population cohort". Psychological Medicine 47 (9): 1659–1667. doi:10.1017/S0033291717000125. PMID 28222824.
- ↑ Cook, A. J. C.; Holliman, Richard; Gilbert, R. E.; Buffolano, W.; Zufferey, J.; Petersen, E.; Jenum, P. A.; Foulon, W. et al. (2000-07-15). "Sources of toxoplasma infection in pregnant women: European multicentre case-control study- Commentary: Congenital toxoplasmosis—further thought for food". BMJ 321 (7254): 142–147. doi:10.1136/bmj.321.7254.142. ISSN 0959-8138. PMID 10894691.
- ↑ Kathleen McAuliffe (March 2012). "How Your Cat is Making You Crazy". The Atlantic. https://www.theatlantic.com/magazine/archive/2012/03/how-your-cat-is-making-you-crazy/8873/.
- ↑ Flegr Jaroslav (2007). "Effects of Toxoplasma on human behavior". Schizophrenia Bulletin 33 (3): 757–760. doi:10.1093/schbul/sbl074. PMID 17218612. PMC 2526142. http://schizophreniabulletin.oxfordjournals.org/content/33/3/757.full.
- ↑ Arthur Ashe, Tennis Star, is Dead at 49 New York Times (02/08/93)
- ↑ Merritt Butrick, A Biography Angelfire.com, accessdate Mar 18, 2011
- ↑ "The Face That Defined AIDS". http://www.broward.org/HumanServices/CommunityPartnerships/RyanWhiteProgram/Pages/TheFaceThatDefinedAIDS.aspx.
- ↑ "Pregnancy superfoods revealed". BBC News. January 10, 2001. http://news.bbc.co.uk/1/hi/health/1109818.stm.
- ↑ "Olympics bid Coes finest race". The Times (London). June 26, 2005. http://www.timesonline.co.uk/tol/sport/article537461.ece.
- ↑ "SPORTS PEOPLE; Coe's Disorder Rare". The New York Times. 3 September 1983. https://www.nytimes.com/1983/09/03/sports/sports-people-coe-s-disorder-rare.html.
- ↑ Brody, Jane E. (27 October 1982). "PERSONAL HEALTH". New York Times. https://www.nytimes.com/1982/10/27/garden/personal-health-247906.html.
- ↑ Rigoulet, Jacques; Hennache, Alain; Lagourette, Pierre; George, Catherine; Longeart, Loïc; Le Net, Jean-Loïc; Dubey, Jitender P. (2014). "Toxoplasmosis in a bar-shouldered dove (Geopelia humeralis) from the Zoo of Clères, France". Parasite 21: 62. doi:10.1051/parasite/2014062. ISSN 1776-1042. PMID 25407506.

- ↑ 111.0 111.1 Ma, Hongyu; Wang, Zedong; Wang, Chengdong; Li, Caiwu; Wei, Feng; Liu, Quan (2015). "Fatal Toxoplasma gondii infection in the giant panda". Parasite 22: 30. doi:10.1051/parasite/2015030. ISSN 1776-1042. PMID 26514595. PMC 4626621. http://www.parasite-journal.org/articles/parasite/full_html/2015/01/parasite150075/parasite150075.html.
- ↑ Dubey (2016), p. needed.
- ↑ Rouatbi, Mariem; Amairia, Safa; Amdouni, Yosra; Boussaadoun, Mohamed Anis; Ayadi, Ouarda; Al-Hosary, Amira Adel Taha; Rekik, Mourad; Ben Abdallah, Rym et al. (2019). "Toxoplasma gondii infection and toxoplasmosis in North Africa: a review". Parasite 26: 6. doi:10.1051/parasite/2019006. ISSN 1776-1042. PMID 30767889.

- ↑ Ekanayake, D. K.; Rajapakse, R. P V. J.; Dubey, J. P.; Dittus, W. P J. (2004). "Seroprevalence of Toxoplasma gondii in wild toque macaques (Macaca sinica) at Polonnaruwa, Sri Lanka". Journal of Parasitology 90 (4): 870–871. doi:10.1645/GE-291R. PMID 15357087.
- ↑ Hollings, Tracey; Jones, Menna; Mooney, Nick; McCallum, Hamish (2013). "Wildlife disease ecology in changing landscapes: Mesopredator release and toxoplasmosis". International Journal for Parasitology: Parasites and Wildlife 2: 110–118. doi:10.1016/j.ijppaw.2013.02.002. PMID 24533323.
- ↑ Fancourt, Bronwyn (5 October 2014). "Toxoplasmosis: how feral cats kill wildlife without lifting a paw". The Conversation. https://theconversation.com/toxoplasmosis-how-feral-cats-kill-wildlife-without-lifting-a-paw-32228.
- ↑ 117.0 117.1 117.2 117.3 Riahi, Mohammad; Fakhri, Yadollah; Hanifehpour, Hooman; Valizadeh, Soghra; Gholizadeh, Majid; Hosseini-Pouya, Rokhsane; Gamble, H.Ray (September 2017). "The global seroprevalence of Toxoplasma gondii among wild boars: A systematic review and meta-analysis". Veterinary Parasitology 244: 12–20. doi:10.1016/j.vetpar.2017.07.013. PMID 28917302.
- ↑ 118.0 118.1 118.2 Dubey, J. P. (2009). "Toxoplasmosis in pigs—The last 20 years". Veterinary Parasitology (Elsevier) 164 (2–4): 89–103. doi:10.1016/j.vetpar.2009.05.018. ISSN 0304-4017. PMID 19559531.
- ↑ Dubey (2016), p. 145.
- ↑ 120.0 120.1 120.2 Nissapatorn, Veeranoot; Lau, Yee-Ling; Fong, Mun-Yik (2013). "Toxoplasma gondii: The Parasite in Trend". in Lim, Yvonne Ai Lian; Vythilingam, Indra. Parasites and their vectors. Vienna: Springer. pp. 155–175. ISBN 978-3-7091-1553-4.
- ↑ "Molecular characterization of Toxoplasma gondii Type II in sheep abortion in Sardinia, Italy". Parasite 21: 6. 2014. doi:10.1051/parasite/2014007. PMID 24534616.

- ↑ 122.0 122.1 122.2 122.3 "Toxoplasma gondii: from animals to humans". International Journal for Parasitology 30 (12–13): 1217–58. November 2000. doi:10.1016/S0020-7519(00)00124-7. PMID 11113252.
- ↑ Dubey (2016), pp. 145–151.
- ↑ Dubey (2016), p. 153.
- ↑ Dubey (2016), p. 154.
- ↑ "High prevalence and abundant atypical genotypes of Toxoplasma gondii isolated from lambs destined for human consumption in the USA". International Journal for Parasitology 38 (8–9): 999–1006. July 2008. doi:10.1016/j.ijpara.2007.11.012. PMID 18191859.
- ↑ "High prevalence and genotypes of Toxoplasma gondii isolated from goats, from a retail meat store, destined for human consumption in the USA". International Journal for Parasitology 41 (8): 827–833. July 2011. doi:10.1016/j.ijpara.2011.03.006. PMID 21515278.
- ↑ Dubey JP (February 2010). "Toxoplasma gondii infections in chickens (Gallus domesticus): prevalence, clinical disease, diagnosis and public health significance". Zoonoses and Public Health 57 (1): 60–73. doi:10.1111/j.1863-2378.2009.01274.x. PMID 19744305.
- ↑ Weiss & Kim (2011), p. 723.
- ↑ Blaga, Radu; Aubert, Dominique; Thébault, Anne; Perret, Catherine; Geers, Régine; Thomas, Myriam; Alliot, Annie; Djokic, Vitomir et al. (2019). "Toxoplasma gondii in beef consumed in France: regional variation in seroprevalence and parasite isolation". Parasite 26: 77. doi:10.1051/parasite/2019076. ISSN 1776-1042. PMID 31868577.

- ↑ Aroussi, Abdelkrim; Vignoles, Philippe; Dalmay, François; Wimel, Laurence; Dardé, Marie-Laure; Mercier, Aurélien; Ajzenberg, Daniel (2015). "Detection of Toxoplasma gondii DNA in horse meat from supermarkets in France and performance evaluation of two serological tests". Parasite 22: 14. doi:10.1051/parasite/2015014. ISSN 1776-1042. PMID 25809058. PMC 4374124. https://www.parasite-journal.org/articles/parasite/full_html/2015/01/parasite150019/parasite150019.html.
- ↑ Dubey, Jitender P. (2008-12-01). "The history of Toxoplasma gondii – the first 100 years". The Journal of Eukaryotic Microbiology 55 (6): 467–475. doi:10.1111/j.1550-7408.2008.00345.x. ISSN 1550-7408. PMID 19120791. https://naldc-legacy.nal.usda.gov/naldc/download.xhtml?id=47190&content=PDF. Retrieved 2018-12-29.
- ↑ Hutchison, W. M. (1965-05-29). "Experimental transmission of Toxoplasma gondii". Nature 206 (987): 961–2. doi:10.1038/206961a0. PMID 5839865. Bibcode: 1965Natur.206..961H.
- ↑ 134.0 134.1 134.2 134.3 "Toxoplasma gondii: epidemiology, feline clinical aspects, and prevention". Trends in Parasitology 26 (4): 190–196. April 2010. doi:10.1016/j.pt.2010.01.009. PMID 20202907. https://digitalcommons.unl.edu/publichealthresources/528.
- ↑ "Feline toxoplasmosis in Finland: cross-sectional epidemiological study and case series study". Journal of Veterinary Diagnostic Investigation 24 (6): 1115–1124. November 2012. doi:10.1177/1040638712461787. PMID 23012380.
- ↑ "High prevalence of toxoplasmosis in cats from Egypt: isolation of viable Toxoplasma gondii, tissue distribution, and isolate designation". The Journal of Parasitology 96 (6): 1115–1118. December 2010. doi:10.1645/GE-2554.1. PMID 21158619.
- ↑ Dubey (2016), p. 96.
- ↑ Dubey (2016), p. 98.
- ↑ Dubey (2016), p. 95.
- ↑ Dubey (2016), p. 46.
- ↑ Andersen, Mark C.; Martin, Brent J.; Roemer, Gary W. (2004-12-15). "Use of matrix population models to estimate the efficacy of euthanasia versus trap-neuter-return for management of free-roaming cats". Journal of the American Veterinary Medical Association 225 (12): 1871–1876. doi:10.2460/javma.2004.225.1871. ISSN 0003-1488. PMID 15643836. https://semanticscholar.org/paper/257a3fdeaddf701df70fbb38aba568bafac3b854.
- ↑ 142.0 142.1 142.2 142.3 "Toxoplasma gondii-altered host behaviour: clues as to mechanism of action". Folia Parasitologica 57 (2): 95–104. June 2010. doi:10.14411/fp.2010.012. PMID 20608471.
- ↑ Webster JP (May 2007). "The effect of Toxoplasma gondii on animal behavior: playing cat and mouse". Schizophrenia Bulletin 33 (3): 752–756. doi:10.1093/schbul/sbl073. PMID 17218613. PMC 2526137. http://schizophreniabulletin.oxfordjournals.org/content/early/2007/01/11/schbul.sbl073.full.pdf.
- ↑ 144.0 144.1 Berdoy, M.; Webster, J. P.; Macdonald, D. W. (August 7, 2000). "Fatal attraction in rats infected with Toxoplasma gondii". Proceedings of the Royal Society B: Biological Sciences 267 (1452): 1591–1594. doi:10.1098/rspb.2000.1182. PMID 11007336.
- ↑ "Behavioral changes induced by Toxoplasma infection of rodents are highly specific to aversion of cat odors". Proceedings of the National Academy of Sciences of the United States of America 104 (15): 6442–6447. April 10, 2007. doi:10.1073/pnas.0608310104. PMID 17404235. Bibcode: 2007PNAS..104.6442V.
- ↑ "Sex-specific changes in gene expression and behavior induced by chronic Toxoplasma infection in mice". Neuroscience 206: 39–48. March 29, 2012. doi:10.1016/j.neuroscience.2011.12.051. PMID 22240252.
- ↑ "Specificity of theToxoplasma gondii-altered behaviour to definitive versus non-definitive host predation risk". Parasitology 135 (10): 1143–1150. September 2008. doi:10.1017/S0031182008004666. PMID 18620624.
- ↑ 148.0 148.1 "Toxoplasma gondii infection reduces predator aversion in rats through epigenetic modulation in the host medial amygdala". Molecular Ecology 23 (24): 6114–6122. December 2014. doi:10.1111/mec.12888. PMID 25142402. Bibcode: 2014MolEc..23.6114H.
- ↑ 149.0 149.1 "Masterpiece of epigenetic engineering – how Toxoplasma gondii reprogrammes host brains to change fear to sexual attraction". Molecular Ecology 23 (24): 5934–5936. December 2014. doi:10.1111/mec.13006. PMID 25532868. Bibcode: 2014MolEc..23.5934F.
- ↑ "The Epigenetic Mechanisms of Amphetamine". Journal of Addiction and Prevention 2015 (S1): 1–7. February 2015. ISSN 2330-2178. PMID 27453897. "Epigenetic modifications caused by addictive drugs play an important role in neuronal plasticity and in drug-induced behavioral responses. Although few studies have investigated the effects of AMPH on gene regulation (Table 1), current data suggest that AMPH acts at multiple levels to alter histone/DNA interaction and to recruit transcription factors which ultimately cause repression of some genes and activation of other genes. Importantly, some studies have also correlated the epigenetic regulation induced by AMPH with the behavioral outcomes caused by this drug, suggesting therefore that epigenetics remodeling underlies the behavioral changes induced by AMPH. If this proves to be true, the use of specific drugs that inhibit histone acetylation, methylation or DNA methylation might be an important therapeutic alternative to prevent and/or reverse AMPH addiction and mitigate the side effects generate by AMPH when used to treat ADHD.".
- ↑ "Regulation of chromatin states by drugs of abuse". Current Opinion in Neurobiology 30: 112–121. February 2015. doi:10.1016/j.conb.2014.11.002. PMID 25486626.
- ↑ "Epigenetic mechanisms of drug addiction". Neuropharmacology 76 (Pt B): 259–268. January 2014. doi:10.1016/j.neuropharm.2013.04.004. PMID 23643695. "Short-term increases in histone acetylation generally promote behavioral responses to the drugs, while sustained increases oppose cocaine's effects, based on the actions of systemic or intra-NAc administration of HDAC inhibitors. ... Genetic or pharmacological blockade of G9a in the NAc potentiates behavioral responses to cocaine and opiates, whereas increasing G9a function exerts the opposite effect (Maze et al., 2010; Sun et al., 2012a). Such drug-induced downregulation of G9a and H3K9me2 also sensitizes animals to the deleterious effects of subsequent chronic stress (Covington et al., 2011). Downregulation of G9a increases the dendritic arborization of NAc neurons, and is associated with increased expression of numerous proteins implicated in synaptic function, which directly connects altered G9a/H3K9me2 in the synaptic plasticity associated with addiction (Maze et al., 2010).
"G9a appears to be a critical control point for epigenetic regulation in NAc, as we know it functions in two negative feedback loops. It opposes the induction of ΔFosB, a long-lasting transcription factor important for drug addiction (Robison and Nestler, 2011), while ΔFosB in turn suppresses G9a expression (Maze et al., 2010; Sun et al., 2012a). ... Also, G9a is induced in NAc upon prolonged HDAC inhibition, which explains the paradoxical attenuation of cocaine's behavioral effects seen under these conditions, as noted above (Kennedy et al., 2013). GABAA receptor subunit genes are among those that are controlled by this feedback loop. Thus, chronic cocaine, or prolonged HDAC inhibition, induces several GABAA receptor subunits in NAc, which is associated with increased frequency of inhibitory postsynaptic currents (IPSCs). In striking contrast, combined exposure to cocaine and HDAC inhibition, which triggers the induction of G9a and increased global levels of H3K9me2, leads to blockade of GABAA receptor and IPSC regulation.
". - ↑ "Toxoplasma histone acetylation remodelers as novel drug targets". Expert Review of Anti-infective Therapy 10 (10): 1189–1201. October 2012. doi:10.1586/eri.12.100. PMID 23199404.
- ↑ "Proteome-wide lysine acetylation in cortical astrocytes and alterations that occur during infection with brain parasite Toxoplasma gondii". PLOS ONE 10 (3): e0117966. 2015. doi:10.1371/journal.pone.0117966. PMID 25786129. Bibcode: 2015PLoSO..1017966B.
- ↑ "Toxoplasma gondii infection and behaviour – location, location, location?". The Journal of Experimental Biology 216 (Pt 1): 113–119. January 1, 2013. doi:10.1242/jeb.074153. PMID 23225873.
- ↑ 156.0 156.1 Hakimi, ed (2012). "Chronic Toxoplasma infection modifies the structure and the risk of host behavior". PLOS ONE 7 (3): e32489. doi:10.1371/journal.pone.0032489. PMID 22431975. Bibcode: 2012PLoSO...732489A.
- ↑ "Toxoplasma gondii infection lower anxiety as measured in the plus-maze and social interaction tests in rats: A behavioral analysis". Behavioural Brain Research 177 (1): 70–79. February 12, 2007. doi:10.1016/j.bbr.2006.11.012. PMID 17169442.
- ↑ "Transmission of Toxoplasma: clues from the study of sea otters as sentinels of Toxoplasma gondii flow into the marine environment". International Journal for Parasitology 35 (11–12): 1155–1168. 2005. doi:10.1016/j.ijpara.2005.07.002. PMID 16157341.
- ↑ "Treating Disease in the Developing World". National Public Radio. December 16, 2005. https://www.npr.org/templates/story/story.php?storyId=5058325.
- ↑ "Parasite in cats killing sea otters". NOAA magazine (National Oceanic and Atmospheric Administration). 21 January 2003. http://www.magazine.noaa.gov/stories/mag72.htm.
- ↑ Diep, Francie (September 3, 2019). "What's Killing California's Sea Otters? House Cats". The New York Times. https://www.nytimes.com/2019/08/28/science/california-sea-otters-cats.html.
- ↑ 162.0 162.1 Dawson, Teresa. "Cat Disease Threatens Endangered Monk Seals". https://www.scientificamerican.com/article/cat-disease-threatens-endangered-monk-seals/.
- ↑ Honnold, S. P.; Braun, R.; Scott, D. P.; Sreekumar, C.; Dubey, J. P. (June 2005). "Toxoplasmosis in a Hawaiian monk seal (Monachus schauinslandi)". Journal of Parasitology 91 (3): 695–697. doi:10.1645/GE-469R. PMID 16108571.
- ↑ "3 Schizophrenia". https://www.newscientist.com/article/mg20427301.600-3-schizophrenia.html.
- ↑ Sidhartha Banerjee (October 15, 2018). "Parasite spread by cats threatens Quebec's endangered belugas(whales)". CBC News.
- ↑ Massie, Gloeta N.; Ware, Michael W.; Villegas, Eric N.; Black, Michael W. (2010). "Uptake and transmission of Toxoplasma gondii oocysts by migratory, filter-feeding fish". Veterinary Parasitology 169 (3–4): 296–303. doi:10.1016/j.vetpar.2010.01.002. ISSN 0304-4017. PMID 20097009.
- ↑ 167.0 167.1 167.2 Fuglewicz, AJ; Piotrowski, P; Stodolak, A (September 2017). "Relationship between toxoplasmosis and schizophrenia: A review". Advances in Clinical and Experimental Medicine 26 (6): 1031–1036. doi:10.17219/acem/61435. PMID 29068607.
- ↑ 168.0 168.1 168.2 168.3 "Toxoplasma gondii infection, from predation to schizophrenia: can animal behaviour help us understand human behaviour?". The Journal of Experimental Biology 216 (Pt 1): 99–112. Jan 1, 2013. doi:10.1242/jeb.074716. PMID 23225872.
- ↑ 169.0 169.1 Flegr J (Jan 1, 2013). "Influence of latent Toxoplasma infection on human personality, physiology and morphology: pros and cons of the Toxoplasma-human model in studying the manipulation hypothesis". The Journal of Experimental Biology 216 (Pt 1): 127–33. doi:10.1242/jeb.073635. PMID 23225875.
- ↑ 170.0 170.1 "Toxoplasmosis gondii and other risk factors for schizophrenia: An update". Schizophrenia Bulletin 38 (3): 642–647. 2012. doi:10.1093/schbul/sbs043. PMID 22446566. PMC 3329973. http://schizophreniabulletin.oxfordjournals.org/content/38/3/642.long.
- ↑ 171.0 171.1 Arias, I; Sorlozano, A; Villegas, E; de Dios Luna, J; McKenney, K; Cervilla, J; Gutierrez, B; Gutierrez, J (April 2012). "Infectious agents associated with schizophrenia: a meta-analysis". Schizophrenia Research 136 (1–3): 128–36. doi:10.1016/j.schres.2011.10.026. PMID 22104141. https://www.researchgate.net/publication/51819116.
- ↑ 172.0 172.1 Flegr J (2013). "How and why toxoplasma makes us crazy". Trends in Parasitology 29 (4): 156–163. doi:10.1016/j.pt.2013.01.007. PMID 23433494.
- ↑ "Schizophrenia and toxoplasmosis". Schizophrenia Bulletin 33 (3): 727–8. May 2007. doi:10.1093/schbul/sbm026. PMID 17426051.
- ↑ de Barros, JLVM; Barbosa, IG; Salem, H; Rocha, NP; Kummer, A; Okusaga, OO; Soares, JC; Teixeira, AL (February 2017). "Is there any association between Toxoplasma gondii infection and bipolar disorder? A systematic review and meta-analysis". Journal of Affective Disorders 209: 59–65. doi:10.1016/j.jad.2016.11.016. PMID 27889597.
- ↑ "The relationship between Toxoplasma gondii infection and mood disorders in the third National Health and Nutrition Survey". Biological Psychiatry 72 (4): 290–5. Aug 15, 2012. doi:10.1016/j.biopsych.2012.01.003. PMID 22325983.
- ↑ Sugden, Karen; Moffitt, Terrie E.; Pinto, Lauriane; Poulton, Richie; Williams, Benjamin S.; Caspi, Avshalom; Tanowitz, Herbert B. (17 February 2016). "Is Toxoplasma Gondii Infection Related to Brain and Behavior Impairments in Humans? Evidence from a Population-Representative Birth Cohort". PLOS ONE 11 (2): e0148435. doi:10.1371/journal.pone.0148435. PMID 26886853. Bibcode: 2016PLoSO..1148435S.
- ↑ "Toxoplasma gondii seropositivity is negatively associated with multiple sclerosis". Journal of Neuroimmunology 285: 119–124. 2015. doi:10.1016/j.jneuroim.2015.05.011. PMID 26198927.
- ↑ Gohardehi, Shaban; Sharif, Mehdi; Sarvi, Shahabeddin; Moosazadeh, Mahmood; Alizadeh-Navaei, Reza; Hosseini, Seyed Abdollah; Amouei, Afsaneh; Pagheh, Abdolsattar et al. (August 2018). "The potential risk of toxoplasmosis for traffic accidents: A systematic review and meta-analysis". Experimental Parasitology 191: 19–24. doi:10.1016/j.exppara.2018.06.003. ISSN 1090-2449. PMID 29906469. https://pubmed.ncbi.nlm.nih.gov/29906469/.
- ↑ 179.0 179.1 179.2 179.3 179.4 Yan, Chao; Liang, Li-Jun; Zheng, Kui-Yang; Zhu, Xing-Quan (2016). "Impact of environmental factors on the emergence, transmission and distribution of Toxoplasma gondii". Parasites & Vectors 9 (137): 137. doi:10.1186/s13071-016-1432-6. PMID 26965989.
- ↑ Dolgin, Elie (March 30, 2017). "Climate change: As the ice melts". Nature 543 (7647): S54–S55. doi:10.1038/543S54a. PMID 28355191. Bibcode: 2017Natur.543S..54D.
- Parts of this article are taken from the public domain CDC factsheet: Toxoplasmosis
Bibliography
- Weiss, L. M.; Kim, K. (28 April 2011). Toxoplasma gondii: The Model Apicomplexan. Perspectives and Methods. Academic Press. ISBN 978-0-08-047501-1. https://books.google.com/books?id=yTUkJEphM_IC. Retrieved 12 March 2013.
- Dubey, J. P. (2016). Toxoplasmosis of Animals and Humans (2nd ed.). Boca Raton: CRC Press. pp. xvii+313. ISBN 978-1-4200-9237-0. OCLC 423572366. https://books.google.com/books?id=5Nm7t5p9APAC. ISBN 1-4200-9236-7 ISBN 9781420092363
- "Structures of Toxoplasma gondii tachyzoites, bradyzoites, and sporozoites and biology and development of tissue cysts". Clinical Microbiology Reviews 11 (2): 267–299. April 1998. doi:10.1128/CMR.11.2.267. PMID 9564564.
- Jaroslav Flegr (2011). Pozor, Toxo!. Academia, Prague, Czech Republic. ISBN 978-80-200-2022-2. http://www.academia.cz/pozor-toxo.html. Retrieved 2014-10-04.
External links
- How a cat-borne parasite infects humans (National Geographic)
- Toxoplasmosis at Merck Manual of Diagnosis and Therapy Professional Edition
- Toxoplasmosis at Health Protection Agency (HPA), United Kingdom
- Pictures of Toxoplasmosis Medical Image Database
- Video-Interview with Professor Robert Sapolsky on Toxoplasmosis and its effect on human behavior (24:27 min)
- "Toxoplasmosis". MedlinePlus. U.S. National Library of Medicine. https://medlineplus.gov/toxoplasmosis.html.
| Classification | |
|---|---|
| External resources |
 |