Chemistry:Butyric acid
|
| |||
| |||
| Names | |||
|---|---|---|---|
| Preferred IUPAC name
Butanoic acid[1] | |||
| Other names
Ethylacetic acid
1-Propanecarboxylic acid Propylformic acid C4:0 (Lipid numbers) | |||
| Identifiers | |||
3D model (JSmol)
|
| ||
| ChEBI |
| ||
| ChEMBL |
| ||
| ChemSpider | |||
| DrugBank |
| ||
| EC Number |
| ||
| |||
| KEGG |
| ||
| MeSH | Butyric+acid | ||
PubChem CID
|
|||
| RTECS number |
| ||
| UNII |
| ||
| UN number | 2820 | ||
| |||
| |||
| Properties | |||
| C3H7COOH | |||
| Molar mass | 88.106 g·mol−1 | ||
| Appearance | Colorless liquid | ||
| Odor | Unpleasant, similar to vomit or body odor | ||
| Density | 1.135 g/cm3 (−43 °C)[2] 0.9528 g/cm3 (25 °C)[3] | ||
| Melting point | −5.1 °C (22.8 °F; 268.0 K)[3] | ||
| Boiling point | 163.75 °C (326.75 °F; 436.90 K)[3] | ||
| Sublimes at −35 °C ΔsublH | |||
| Miscible | |||
| Solubility | Miscible with ethanol, ether. Slightly soluble in CCl4 | ||
| log P | 0.79 | ||
| Vapor pressure | 0.112 kPa (20 °C) 0.74 kPa (50 °C) 9.62 kPa (100 °C)[4] | ||
Henry's law
constant (kH) |
5.35·10−4 L·atm/mol | ||
| Acidity (pKa) | 4.82 | ||
| −55.10·10−6 cm3/mol | |||
| Thermal conductivity | 1.46·105 W/m·K | ||
Refractive index (nD)
|
1.398 (20 °C)[3] | ||
| Viscosity | 1.814 cP (15 °C)[5] 1.426 cP (25 °C) | ||
| Structure | |||
| Monoclinic (−43 °C)[2] | |||
| C2/m[2] | |||
a = 8.01 Å, b = 6.82 Å, c = 10.14 Å[2] α = 90°, β = 111.45°, γ = 90°
| |||
| 0.93 D (20 °C)[5] | |||
| Thermochemistry | |||
Heat capacity (C)
|
178.6 J/mol·K[4] | ||
Std molar
entropy (S |
222.2 J/mol·K[5] | ||
Std enthalpy of
formation (ΔfH⦵298) |
−533.9 kJ/mol[4] | ||
Std enthalpy of
combustion (ΔcH⦵298) |
2183.5 kJ/mol[4] | ||
| Hazards | |||
| Safety data sheet | External MSDS | ||
| GHS pictograms |  [6] [6]
| ||
| GHS Signal word | Danger | ||
| H314[6] | |||
| P280, P305+351+338, P310[6] | |||
| NFPA 704 (fire diamond) | |||
| Flash point | 71 to 72 °C (160 to 162 °F; 344 to 345 K)[6] | ||
| 440 °C (824 °F; 713 K)[6] | |||
| Explosive limits | 2.2–13.4% | ||
| Lethal dose or concentration (LD, LC): | |||
LD50 (median dose)
|
2000 mg/kg (oral, rat) | ||
| Related compounds | |||
Related carboxylic acids
|
Propionic acid, Pentanoic acid | ||
Related compounds
|
1-Butanol Butyraldehyde Methyl butyrate | ||
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |||
| Infobox references | |||
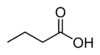
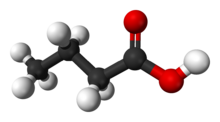
Butyric acid (/ˈbjuːtɪrɪk/; from Ancient Greek:, meaning "butter"), also known under the systematic name butanoic acid, is a straight-chain alkyl carboxylic acid with the chemical formula CH
3CH
2CH
2CO
2H. It is an oily, colorless liquid with an unpleasant odor. Isobutyric acid (2-methylpropanoic acid) is an isomer. Salts and esters of butyric acid are known as butyrates or butanoates. The acid does not occur widely in nature, but its esters are widespread. It is a common industrial chemical[7] and an important component in the mammalian gut.
History
Butyric acid was first observed in an impure form in 1814 by the French chemist Michel Eugène Chevreul. By 1818, he had purified it sufficiently to characterize it. However, Chevreul did not publish his early research on butyric acid; instead, he deposited his findings in manuscript form with the secretary of the Academy of Sciences in Paris, France. Henri Braconnot, a French chemist, was also researching the composition of butter and was publishing his findings and this led to disputes about priority. As early as 1815, Chevreul claimed that he had found the substance responsible for the smell of butter.[8] By 1817, he published some of his findings regarding the properties of butyric acid and named it.[9] However, it was not until 1823 that he presented the properties of butyric acid in detail.[10] The name butyric acid comes from βούτῡρον, meaning "butter", the substance in which it was first found. The Latin name butyrum (or buturum) is similar.
Occurrence
Triglycerides of butyric acid compose 3–4% of butter. When butter goes rancid, butyric acid is liberated from the glyceride by hydrolysis.[11] It is one of the fatty acid subgroup called short-chain fatty acids. Butyric acid is a typical carboxylic acid that reacts with bases and affects many metals.[12] It is found in animal fat and plant oils, bovine milk, breast milk, butter, parmesan cheese, body odor, vomit and as a product of anaerobic fermentation (including in the colon).[13][14] It has a taste somewhat like butter and an unpleasant odor. Mammals with good scent detection abilities, such as dogs, can detect it at 10 parts per billion, whereas humans can detect it only in concentrations above 10 parts per million. In food manufacturing, it is used as a flavoring agent.[15]
In humans, butyric acid is one of two primary endogenous agonists of human hydroxycarboxylic acid receptor 2 (HCA
2), a Gi/o-coupled G protein-coupled receptor.[16][17]
Butyric acid is present as its octyl ester in parsnip (Pastinaca sativa)[18] and in the seed of the ginkgo tree.[19]
Production
Industrial
In industry, butyric acid is produced by hydroformylation from propene and syngas, forming butyraldehyde, which is oxidised to the final product.[7]
- H
2 + CO + CH
3CH=CH
2 → CH
3CH
2CH
2CHObutyric acid
It can be separated from aqueous solutions by saturation with salts such as calcium chloride. The calcium salt, Ca(C
4H
7O
2)
2 · H
2O, is less soluble in hot water than in cold.
Microbial biosynthesis
Butyrate is produced by several fermentation processes performed by obligate anaerobic bacteria.[20] This fermentation pathway was discovered by Louis Pasteur in 1861. Examples of butyrate-producing species of bacteria:
- Clostridium butyricum
- Clostridium kluyveri
- Clostridium pasteurianum
- Faecalibacterium prausnitzii
- Fusobacterium nucleatum
- Butyrivibrio fibrisolvens
- Eubacterium limosum
The pathway starts with the glycolytic cleavage of glucose to two molecules of pyruvate, as happens in most organisms. Pyruvate is oxidized into acetyl coenzyme A catalyzed by pyruvate:ferredoxin oxidoreductase. Two molecules of carbon dioxide (CO
2) and two molecules of hydrogen (H
2) are formed as waste products. Subsequently, ATP is produced in the last step of the fermentation. Three molecules of ATP are produced for each glucose molecule, a relatively high yield. The balanced equation for this fermentation is
- C
6H
12O
6 → C
4H
8O
2 + 2CO
2 + 2H
2
Other pathways to butyrate include succinate reduction and crotonate disproportionation.
| Action | Responsible enzyme |
|---|---|
| Acetyl coenzyme A converts into acetoacetyl coenzyme A | acetyl-CoA-acetyl transferase |
| Acetoacetyl coenzyme A converts into β-hydroxybutyryl CoA | β-hydroxybutyryl-CoA dehydrogenase |
| β-hydroxybutyryl CoA converts into crotonyl CoA | crotonase |
| Crotonyl CoA converts into butyryl CoA (CH 3CH 2CH 2C=O–CoA) |
butyryl CoA dehydrogenase |
| A phosphate group replaces CoA to form butyryl phosphate | phosphobutyrylase |
| The phosphate group joins ADP to form ATP and butyrate | butyrate kinase |
Several species form acetone and n-butanol in an alternative pathway, which starts as butyrate fermentation. Some of these species are:
- Clostridium acetobutylicum, the most prominent acetone and butanol producer, used also in industry
- Clostridium beijerinckii
- Clostridium tetanomorphum
- Clostridium aurantibutyricum
These bacteria begin with butyrate fermentation, as described above, but, when the pH drops below 5, they switch into butanol and acetone production to prevent further lowering of the pH. Two molecules of butanol are formed for each molecule of acetone.
The change in the pathway occurs after acetoacetyl CoA formation. This intermediate then takes two possible pathways:
- acetoacetyl CoA → acetoacetate → acetone
- acetoacetyl CoA → butyryl CoA → butyraldehyde → butanol
Fermentable fiber sources
Highly-fermentable fiber residues, such as those from resistant starch, oat bran, pectin, and guar are transformed by colonic bacteria into short-chain fatty acids (SCFA) including butyrate, producing more SCFA than less fermentable fibers such as celluloses.[14][21] One study found that resistant starch consistently produces more butyrate than other types of dietary fiber.[22] The production of SCFA from fibers in ruminant animals such as cattle is responsible for the butyrate content of milk and butter.[13][23]
Fructans are another source of prebiotic soluble dietary fibers which can be digested to produce butyrate.[24] They are often found in the soluble fibers of foods which are high in sulfur, such as the allium and cruciferous vegetables. Sources of fructans include wheat (although some wheat strains such as spelt contain lower amounts),[25] rye, barley, onion, garlic, Jerusalem and globe artichoke, asparagus, beetroot, chicory, dandelion leaves, leek, radicchio, the white part of spring onion, broccoli, brussels sprouts, cabbage, fennel, and prebiotics, such as fructooligosaccharides (FOS), oligofructose, and inulin.[26][27]
Reactions
Butyric acid reacts as a typical carboxylic acid: it can form amide, ester, anhydride, and chloride derivatives.[28] The latter, butyryl chloride, is commonly used as the intermediate to obtain the others.
Uses
Butyric acid is used in the preparation of various butyrate esters. It is used to produce cellulose acetate butyrate (CAB), which is used in a wide variety of tools, paints, and coatings, and is more resistant to degradation than cellulose acetate.[29] CAB can degrade with exposure to heat and moisture, releasing butyric acid.[30]
Low-molecular-weight esters of butyric acid, such as methyl butyrate, have mostly pleasant aromas or tastes.[7] As a consequence, they are used as food and perfume additives. It is an approved food flavoring in the EU FLAVIS database (number 08.005).
Due to its powerful odor, it has also been used as a fishing bait additive.[31] Many of the commercially available flavors used in carp (Cyprinus carpio) baits use butyric acid as their ester base. It is not clear whether fish are attracted by the butyric acid itself or the substances added to it. Butyric acid was one of the few organic acids shown to be palatable for both tench and bitterling.[32] The substance has been used as a stink bomb by the Sea Shepherd Conservation Society to disrupt Japanese whaling crews.[33]
Pharmacology
| Inhibited enzyme | IC50 (nM) | Entry note |
|---|---|---|
| HDAC1 | 16,000 | |
| HDAC2 | 12,000 | |
| HDAC3 | 9,000 | |
| HDAC4 | 2,000,000 | Lower bound |
| HDAC5 | 2,000,000 | Lower bound |
| HDAC6 | 2,000,000 | Lower bound |
| HDAC7 | 2,000,000 | Lower bound |
| HDAC8 | 15,000 | |
| HDAC9 | 2,000,000 | Lower bound |
| CA1 | 511,000 | |
| CA2 | 1,032,000 | |
| GPCR target | pEC50 | Entry note |
| FFAR2 | 2.9–4.6 | Full agonist |
| FFAR3 | 3.8–4.9 | Full agonist |
| HCA 2 |
2.8 | Agonist |
Pharmacodynamics
Butyric acid (pKa 4.82) is fully ionized at physiological pH, so its anion is the material that is mainly relevant in biological systems.
It is one of two primary endogenous agonists of human hydroxycarboxylic acid receptor 2 (HCA
2, also known as GPR109A), a Gi/o-coupled G protein-coupled receptor (GPCR),[16][17]
Like other short-chain fatty acids (SCFAs), butyrate is an agonist at the free fatty acid receptors FFAR2 and FFAR3, which function as nutrient sensors that facilitate the homeostatic control of energy balance; however, among the group of SCFAs, only butyrate is an agonist of HCA2.[36][37][38] It is also an HDAC inhibitor (specifically, HDAC1, HDAC2, HDAC3, and HDAC8),[34][35] a drug that inhibits the function of histone deacetylase enzymes, thereby favoring an acetylated state of histones in cells.[38] Histone acetylation loosens the structure of chromatin by reducing the electrostatic attraction between histones and DNA.[38] In general, it is thought that transcription factors will be unable to access regions where histones are tightly associated with DNA (i.e., non-acetylated, e.g., heterochromatin). Therefore, butyric acid is thought to enhance the transcriptional activity at promoters,[38] which are typically silenced or downregulated due to histone deacetylase activity.
Pharmacokinetics
Butyrate that is produced in the colon through microbial fermentation of dietary fiber is primarily absorbed and metabolized by colonocytes and the liver[note 1] for the generation of ATP during energy metabolism; however, some butyrate is absorbed in the distal colon, which is not connected to the portal vein, thereby allowing for the systemic distribution of butyrate to multiple organ systems through the circulatory system.[dubious ][38] Butyrate that has reached systemic circulation can readily cross the blood–brain barrier via monocarboxylate transporters (i.e., certain members of the SLC16A group of transporters).[39][40] Other transporters that mediate the passage of butyrate across lipid membranes include SLC5A8 (SMCT1), SLC27A1 (FATP1), and SLC27A4 (FATP4).[34][40]
Metabolism
Butyric acid is metabolized by various human XM-ligases (ACSM1, ACSM2B, ASCM3, ACSM4, ACSM5, and ACSM6), also known as butyrate–CoA ligase.[41][42] The metabolite produced by this reaction is butyryl–CoA, and is produced as follows:[41]
- Adenosine triphosphate + butyric acid + coenzyme A → adenosine monophosphate + pyrophosphate + butyryl-CoA
As a short-chain fatty acid, butyrate is metabolized by mitochondria as an energy (i.e., adenosine triphosphate or ATP) source through fatty acid metabolism.[38] In particular, it is an important energy source for cells lining the mammalian colon (colonocytes).[24] Without butyrates, colon cells undergo autophagy (i.e., self-digestion) and die.[43]
In humans, the butyrate precursor tributyrin, which is naturally present in butter, is metabolized by triacylglycerol lipase into dibutyrin and butyrate through the reaction:[44]
- Tributyrin + H
2O → dibutyrin + butyric acid
Biochemistry
Butyrate has numerous effects on energy homeostasis and related diseases (diabetes and obesity), inflammation, and immune function (e.g., it has pronounced antimicrobial and anticarcinogenic effects) in humans. These effects occur through its metabolism by mitochondria to generate ATP during fatty acid metabolism or through one or more of its histone-modifying enzyme targets (i.e., the class I histone deacetylases) and G-protein coupled receptor targets (i.e., FFAR2, FFAR3, and HCA
2).[36][45]
In the mammalian gut
Butyrate is essential to host immune homeostasis.[36] Although the role and importance of butyrate in the gut is not fully understood, many researchers argue that a depletion of butyrate-producing bacteria in patients with several vasculitic conditions is essential to the pathogenesis of these disorders. A depletion of butyrate in the gut is typically caused by an absence or depletion of butyrate-producing-bacteria (BPB). This depletion in BPB leads to microbial dysbiosis. This is characterized by an overall low biodiversity and a depletion of key butyrate-producing members. Butyrate is an essential microbial metabolite with a vital role as a modulator of proper immune function in the host. It has been shown that children lacking in BPB are more susceptible to allergic disease[46] and Type 1 Diabetes.[47] Butyrate is also reduced in a diet low in dietary fiber, which can induce inflammation and have other adverse affects insofar as these short-chain fatty acids activate PPAR-γ.[48]
Butyrate exerts a key role for the maintenance of immune homeostasis both locally (in the gut) and systemically (via circulating butyrate). It has been shown to promote the differentiation of regulatory T cells. In particular, circulating butyrate prompts the generation of extrathymic regulatory T cells. The low-levels of butyrate in human subjects could favor reduced regulatory T cell-mediated control, thus promoting a powerful immuno-pathological T-cell response.[49] On the other hand, gut butyrate has been reported to inhibit local pro-inflammatory cytokines. The absence or depletion of these BPB in the gut could therefore be a possible aide in the overly-active inflammatory response. Butyrate in the gut also protects the integrity of the intestinal epithelial barrier. Decreased butyrate levels therefore lead to a damaged or dysfunctional intestinal epithelial barrier.[50]
In a 2013 research study conducted by Furusawa et al., microbe-derived butyrate was found to be essential in inducing the differentiation of colonic regulatory T cells in mice. This is of great importance and possibly relevant to the pathogenesis and vasculitis associated with many inflammatory diseases because regulatory T cells have a central role in the suppression of inflammatory and allergic responses.[51] In several research studies, it has been demonstrated that butyrate induced the differentiation of regulatory T cells in vitro and in vivo.[52] The anti-inflammatory capacity of butyrate has been extensively analyzed and supported by many studies. It has been found that microorganism-produced butyrate expedites the production of regulatory T cells, although the specific mechanism by which it does so unclear.[53] More recently, it has been shown that butyrate plays an essential and direct role in modulating gene expression of cytotoxic T-cells.[54] Butyrate also has an anti-inflammatory effect on neutrophils, reducing their migration to wounds. This effect is mediated via the receptor HCA
1[55]
In the gut microbiomes found in the class Mammalia, omnivores and herbivores have butyrate-producing bacterial communities dominated by the butyryl-CoA:acetate CoA-transferase pathway, whereas carnivores have butyrate-producing bacterial communities dominated by the butyrate kinase pathway.[56]
Immunomodulation and inflammation
Butyrate's effects on the immune system are mediated through the inhibition of class I histone deacetylases and activation of its G-protein coupled receptor targets: HCA
2 (GPR109A), FFAR2 (GPR43), and FFAR3 (GPR41).[37][57] Among the short-chain fatty acids, butyrate is the most potent promoter of intestinal regulatory T cells in vitro and the only one among the group that is an HCA
2 ligand.[37] It has been shown to be a critical mediator of the colonic inflammatory response. It possesses both preventive and therapeutic potential to counteract inflammation-mediated ulcerative colitis and colorectal cancer.
Butyrate has established antimicrobial properties in humans that are mediated through the antimicrobial peptide LL-37, which it induces via HDAC inhibition on histone H3.[57][58][59] In vitro, butyrate increases gene expression of FOXP3 (the transcription regulator for Tregs) and promotes colonic regulatory T cells (Tregs) through the inhibition of class I histone deacetylases;[37][57] through these actions, it increases the expression of interleukin 10, an anti-inflammatory cytokine.[57][37] Butyrate also suppresses colonic inflammation by inhibiting the IFN-γ–STAT1 signaling pathways, which is mediated partially through histone deacetylase inhibition. While transient IFN-γ signaling is generally associated with normal host immune response, chronic IFN-γ signaling is often associated with chronic inflammation. It has been shown that butyrate inhibits activity of HDAC1 that is bound to the Fas gene promoter in T cells, resulting in hyperacetylation of the Fas promoter and up-regulation of Fas receptor on the T-cell surface.[60]
Similar to other HCA
2 agonists studied, butyrate also produces marked anti-inflammatory effects in a variety of tissues, including the brain, gastrointestinal tract, skin, and vascular tissue.[61][62][63] Butyrate binding at FFAR3 induces neuropeptide Y release and promotes the functional homeostasis of colonic mucosa and the enteric immune system.[64]
Cancer
Butyrate has been shown to be a critical mediator of the colonic inflammatory response. It is responsible for about 70% of energy from the colonocytes, being a critical SCFA in colon homeostasis.[65] Butyrate possesses both preventive and therapeutic potential to counteract inflammation-mediated ulcerative colitis (UC) and colorectal cancer.[66] It produces different effects in healthy and cancerous cells: this is known as the "butyrate paradox". In particular, butyrate inhibits colonic tumor cells and stimulates proliferation of healthy colonic epithelial cells.[67][68] The explanation why butyrate is an energy source for normal colonocytes and induces apoptosis in colon cancer cells, is the Warburg effect in cancer cells, which leads to butyrate not being properly metabolized. This phenomenon leads to the accumulation of butyrate in the nucleus, acting as a histone deacetylase (HDAC) inhibitor.[69] One mechanism underlying butyrate function in suppression of colonic inflammation is inhibition of the IFN-γ/STAT1 signalling pathways. It has been shown that butyrate inhibits activity of HDAC1 that is bound to the Fas gene promoter in T cells, resulting in hyperacetylation of the Fas promoter and upregulation of Fas receptor on the T cell surface. It is thus suggested that butyrate enhances apoptosis of T cells in the colonic tissue and thereby eliminates the source of inflammation (IFN-γ production).[70] Butyrate inhibits angiogenesis by inactivating Sp1 transcription factor activity and downregulating vascular endothelial growth factor gene expression.[71]
In summary, the production of volatile fatty acids such as butyrate from fermentable fibers may contribute to the role of dietary fiber in colon cancer. Short-chain fatty acids, which include butyric acid, are produced by beneficial colonic bacteria (probiotics) that feed on, or ferment prebiotics, which are plant products that contain dietary fiber. These short-chain fatty acids benefit the colonocytes by increasing energy production, and may protect against colon cancer by inhibiting cell proliferation.[21]
Conversely, some researchers have sought to eliminate butyrate and consider it a potential cancer driver.[72] Studies in mice indicate it drives transformation of MSH2-deficient colon epithelial cells.[73]
Potential treatments from butyrate restoration
Owing to the importance of butyrate as an inflammatory regulator and immune system contributor, butyrate depletions could be a key factor influencing the pathogenesis of many vasculitic conditions. It is thus essential to maintain healthy levels of butyrate in the gut. Fecal microbiota transplants (to restore BPB and symbiosis in the gut) could be effective by replenishing butyrate levels. In this treatment, a healthy individual donates their stool to be transplanted into an individual with dysbiosis. A less-invasive treatment option is the administration of butyrate—as oral supplements or enemas—which has been shown to be very effective in terminating symptoms of inflammation with minimal-to-no side-effects. In a study where patients with ulcerative colitis were treated with butyrate enemas, inflammation decreased significantly, and bleeding ceased completely after butyrate provision.[74]
Addiction
Butyric acid is an HDAC inhibitor that is selective for class I HDACs in humans.[34] HDACs are histone-modifying enzymes that can cause histone deacetylation and repression of gene expression. HDACs are important regulators of synaptic formation, synaptic plasticity, and long-term memory formation. Class I HDACs are known to be involved in mediating the development of an addiction.[75][76][77] Butyric acid and other HDAC inhibitors have been used in preclinical research to assess the transcriptional, neural, and behavioral effects of HDAC inhibition in animals addicted to drugs.[77][78][79]
Butyrate salts and esters
The butyrate or butanoate ion, C
3H
7COO−
, is the conjugate base of butyric acid. It is the form found in biological systems at physiological pH. A butyric (or butanoic) compound is a carboxylate salt or ester of butyric acid.
Examples
Salts
Esters
- Butyl butyrate
- Butyryl-CoA
- Cellulose acetate butyrate (aircraft dope)
- Estradiol benzoate butyrate
- Ethyl butyrate
- Methyl butyrate
- Pentyl butyrate
- Tributyrin
See also
- List of saturated fatty acids
- Hershey's milk chocolate
- Histone
- Histone-modifying enzyme
- Histone acetylase
- Histone deacetylase
- Histone-modifying enzyme
- Hydroxybutyric acids
- α-Hydroxybutyric acid
- β-Hydroxybutyric acid
- γ-Hydroxybutyric acid
- Oxobutyric acids
- 2-Oxobutyric acid (α-ketobutyric acid)
- 3-Oxobutyric acid (acetoacetic acid)
- 4-Oxobutyric acid (succinic semialdehyde)
- β-Methylbutyric acid
Notes
- ↑ Most of the butyrate that is absorbed into blood plasma from the colon enters the circulatory system via the portal vein; most of the butyrate that enters the circulatory system by this route is taken up by the liver.[38]
References
- ↑ "Applications to Specific Classes of Compounds". Nomenclature of Organic Chemistry : IUPAC Recommendations and Preferred Names 2013 (Blue Book). Cambridge: The Royal Society of Chemistry. 2014. p. 746. doi:10.1039/9781849733069-00648. ISBN 978-0-85404-182-4.
- ↑ 2.0 2.1 2.2 2.3 Strieter, F. J.; Templeton, D. H. (1962). "Crystal structure of butyric acid". Acta Crystallographica 15 (12): 1240–1244. doi:10.1107/S0365110X6200328X. Bibcode: 1962AcCry..15.1240S. https://escholarship.org/content/qt2576b18r/qt2576b18r.pdf?t=p0llqf.
- ↑ 3.0 3.1 3.2 3.3 Lide, David R., ed (2009). CRC Handbook of Chemistry and Physics (90th ed.). Boca Raton, Florida: CRC Press. ISBN 978-1-4200-9084-0.
- ↑ 4.0 4.1 4.2 4.3 4.4 Butanoic acid in Linstrom, Peter J.; Mallard, William G. (eds.); NIST Chemistry WebBook, NIST Standard Reference Database Number 69, National Institute of Standards and Technology, Gaithersburg (MD), http://webbook.nist.gov (retrieved 27 October 2020)
- ↑ 5.0 5.1 5.2 "Butanoic acid". Chemister.ru. 2007-03-19. http://chemister.ru/Database/properties-en.php?dbid=1&id=1985.
- ↑ 6.0 6.1 6.2 6.3 6.4 Sigma-Aldrich Co., Butyric acid. Retrieved on 27 October 2020.
- ↑ 7.0 7.1 7.2 Riemenschneider, Wilhelm (2002). "Ullmann's Encyclopedia of Industrial Chemistry". Ullmann's Encyclopedia of Industrial Chemistry. Weinheim: Wiley-VCH. doi:10.1002/14356007.a05_235.
- ↑ Chevreul (1815) "Lettre de M. Chevreul à MM. les rédacteurs des Annales de chimie" (Letter from Mr. Chevreul to the editors of the Annals of Chemistry), Annales de chimie, 94 : 73–79; in a footnote spanning pages 75–76, he mentions that he had found a substance that is responsible for the smell of butter.
- ↑ Chevreul (1817) "Extrait d'une lettre de M. Chevreul à MM. les Rédacteurs du Journal de Pharmacie" (Extract of a letter from Mr. Chevreul to the editors of the Journal of Pharmacy), Journal de Pharmacie et des sciences accessoires, 3 : 79–81. On p. 81, he named butyric acid: "Ce principe, que j'ai appelé depuis acid butérique, … " (This principle [i.e., constituent], which I have since named "butyric acid", … )
- ↑ E. Chevreul, Recherches chimiques sur les corps gras d'origine animale [Chemical researches on fatty substances of animal origin] (Paris, France: F.G. Levrault, 1823), pages 115–133.
- ↑ Woo, A.H.; Lindsay, R.C. (1983). "Stepwise Discriminant Analysis of Free Fatty Acid Profiles for Identifying Sources of Lipolytic Enzymes in Rancid Butter". Journal of Dairy Science 66 (10): 2070–2075. doi:10.3168/jds.S0022-0302(83)82052-9.
- ↑ ICSC 1334 – Butyric acid. Inchem.org (23 November 1998). Retrieved on 2020-10-27.
- ↑ 13.0 13.1 McNabney, S. M.; Henagan, T. M. (2017). "Short Chain Fatty Acids in the Colon and Peripheral Tissues: A Focus on Butyrate, Colon Cancer, Obesity and Insulin Resistance". Nutrients 9 (12): 1348. doi:10.3390/nu9121348. PMID 29231905.
- ↑ 14.0 14.1 Morrison, D. J.; Preston, T. (2016). "Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism". Gut Microbes 7 (3): 189–200. doi:10.1080/19490976.2015.1134082. PMID 26963409.
- ↑ "Butyric acid". http://www.thegoodscentscompany.com/data/rw1003411.html.
- ↑ 16.0 16.1 "International Union of Basic and Clinical Pharmacology. LXXXII: Nomenclature and Classification of Hydroxy-carboxylic Acid Receptors (GPR81, GPR109A, and GPR109B)". Pharmacological Reviews 63 (2): 269–90. June 2011. doi:10.1124/pr.110.003301. PMID 21454438.
- ↑ 17.0 17.1 "Hydroxycarboxylic acid receptors". International Union of Basic and Clinical Pharmacology. http://www.guidetopharmacology.org/GRAC/FamilyDisplayForward?familyId=48.
- ↑ Carroll, Mark J.; Berenbaum, May R. (2002). "Behavioral responses of the parsnip webworm to host plant volatiles". Journal of Chemical Ecology 28 (11): 2191–2201. doi:10.1023/A:1021093114663. PMID 12523562.
- ↑ Raven, Peter H.; Evert, Ray F.; Eichhorn, Susan E. (2005). Biology of Plants. W. H. Freemanand Company. pp. 429–431. ISBN 978-0-7167-1007-3. https://archive.org/details/biologyofplants00rave_0. Retrieved 11 October 2018.
- ↑ Seedorf, H.; Fricke, W. F.; Veith, B.; Bruggemann, H.; Liesegang, H.; Strittmatter, A.; Miethke, M.; Buckel, W. et al. (2008). "The Genome of Clostridium kluyveri, a Strict Anaerobe with Unique Metabolic Features". Proceedings of the National Academy of Sciences 105 (6): 2128–2133. doi:10.1073/pnas.0711093105. PMID 18218779. Bibcode: 2008PNAS..105.2128S.
- ↑ 21.0 21.1 "Microbial degradation products influence colon cancer risk: the butyrate controversy". The Journal of Nutrition 134 (2): 479–82. February 2004. doi:10.1093/jn/134.2.479. PMID 14747692.
- ↑ "Prebiotic digestion and fermentation". The American Journal of Clinical Nutrition 73 (2 Suppl): 415S–420S. February 2001. doi:10.1093/ajcn/73.2.415s. PMID 11157351.
- ↑ "Effect of feed on the composition of milk fat". Journal of Dairy Science 74 (9): 3244–57. September 1991. doi:10.3168/jds.S0022-0302(91)78510-X. PMID 1779073.
- ↑ 24.0 24.1 Rivière, Audrey; Selak, Marija; Lantin, David; Leroy, Frédéric; De Vuyst, Luc (2016). "Bifidobacteria and Butyrate-Producing Colon Bacteria: Importance and Strategies for Their Stimulation in the Human Gut". Frontiers in Microbiology 7: 979. doi:10.3389/fmicb.2016.00979. PMID 27446020.
- ↑ "Frequently asked questions in the area of diet and IBS". Department of Gastroenterology Translational Nutrition Science, Monash University, Victoria, Australia. http://www.med.monash.edu/cecs/gastro/fodmap/diet-and-ibs.html#5.
- ↑ Gibson, Peter R.; Shepherd, Susan J. (1 February 2010). "Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach". Journal of Gastroenterology and Hepatology 25 (2): 252–258. doi:10.1111/j.1440-1746.2009.06149.x. ISSN 1440-1746. PMID 20136989.
- ↑ Gibson, Peter R.; Varney, Jane; Malakar, Sreepurna; Muir, Jane G. (1 May 2015). "Food components and irritable bowel syndrome". Gastroenterology 148 (6): 1158–1174.e4. doi:10.1053/j.gastro.2015.02.005. ISSN 1528-0012. PMID 25680668.
- ↑ Jenkins, P. R. (1985). "Carboxylic acids and derivatives". General and Synthetic Methods. 7. pp. 96–160. doi:10.1039/9781847556196-00096. ISBN 978-0-85186-884-4.
- ↑ Lokensgard, Erik (2015). Industrial Plastics: Theory and Applications (6th ed.). Cengage Learning.
- ↑ Williams, R. Scott. "Care of Plastics: Malignant plastics". WAAC Newsletter (Conservation OnLine) 24 (1). http://cool.conservation-us.org/waac/wn/wn24/wn24-1/wn24-102.html.
- ↑ Freezer Baits , nutrabaits.net
- ↑ Kasumyan, A.O.; Døving, K.B. (2003). "Taste preferences in fishes". Fish and Fisheries 4 (4): 289–347. doi:10.1046/j.1467-2979.2003.00121.x. Bibcode: 2003AqFF....4..289K.
- ↑ Japanese Whalers Injured by Acid-Firing Activists , newser.com, 10 February 2010
- ↑ 34.0 34.1 34.2 34.3 "Butyric acid". International Union of Basic and Clinical Pharmacology. http://www.guidetopharmacology.org/GRAC/LigandDisplayForward?tab=biology&ligandId=1059.
- ↑ 35.0 35.1 "Butanoic acid and Sodium butyrate". The Binding Database. http://www.bindingdb.org/bind/searchby_smiles.jsp?submit=Search&startPg=0&Increment=15&SearchType=3&smilesStr=CCCC%28%5BO-%5D%29%3DO&molfile=CCCC%28%5BO-%5D%29%3DO&Similarity=.99.
- ↑ 36.0 36.1 36.2 "Dietary gut microbial metabolites, short-chain fatty acids, and host metabolic regulation". Nutrients 7 (4): 2839–49. 2015. doi:10.3390/nu7042839. PMID 25875123. "Short-chain fatty acids (SCFAs) such as acetate, butyrate, and propionate, which are produced by gut microbial fermentation of dietary fiber, are recognized as essential host energy sources and act as signal transduction molecules via G-protein coupled receptors (FFAR2, FFAR3, OLFR78, GPR109A) and as epigenetic regulators of gene expression by the inhibition of histone deacetylase (HDAC). Recent evidence suggests that dietary fiber and the gut microbial-derived SCFAs exert multiple beneficial effects on the host energy metabolism not only by improving the intestinal environment, but also by directly affecting various host peripheral tissues.".
- ↑ 37.0 37.1 37.2 37.3 37.4 "The environment of regulatory T cell biology: cytokines, metabolites, and the microbiome". Front Immunol 6: 61. February 2015. doi:10.3389/fimmu.2015.00061. PMID 25741338.
Figure 1: Microbial-derived molecules promote colonic Treg differentiation. - ↑ 38.0 38.1 38.2 38.3 38.4 38.5 38.6 "Butyrate, neuroepigenetics and the gut microbiome: Can a high fiber diet improve brain health?". Neurosci. Lett. 625: 56–63. June 2016. doi:10.1016/j.neulet.2016.02.009. PMID 26868600.
- ↑ "Small molecular drug transfer across the blood–brain barrier via carrier-mediated transport systems". NeuroRx 2 (1): 54–62. 2005. doi:10.1602/neurorx.2.1.54. PMID 15717057. "Other in vivo studies in our laboratories indicated that several compounds including acetate, propionate, butyrate, benzoic acid, salicylic acid, nicotinic acid, and some β-lactam antibiotics may be transported by the MCT at the BBB.21 ... Uptake of valproic acid was reduced in the presence of medium-chain fatty acids such as hexanoate, octanoate, and decanoate, but not propionate or butyrate, indicating that valproic acid is taken up into the brain via a transport system for medium-chain fatty acids, not short-chain fatty acids.".
- ↑ 40.0 40.1 "Role of monocarboxylate transporters in drug delivery to the brain". Curr. Pharm. Des. 20 (10): 1487–98. 2014. doi:10.2174/13816128113199990462. PMID 23789956. "Monocarboxylate transporters (MCTs) are known to mediate the transport of short chain monocarboxylates such as lactate, pyruvate and butyrate. ... MCT1 and MCT4 have also been associated with the transport of short chain fatty acids such as acetate and formate which are then metabolized in the astrocytes [78]. ... SLC5A8 is expressed in normal colon tissue, and it functions as a tumor suppressor in human colon with silencing of this gene occurring in colon carcinoma. This transporter is involved in the concentrative uptake of butyrate and pyruvate produced as a product of fermentation by colonic bacteria.".
- ↑ 41.0 41.1 "Butyric acid". Butyric acid. University of Alberta. http://www.hmdb.ca/metabolites/HMDB00039. Retrieved 15 August 2015.
- ↑ "Butanoate metabolism – Reference pathway". Kanehisa Laboratories. 1 November 2017. http://www.genome.jp/kegg-bin/show_pathway?map00650.
- ↑ Donohoe, Dallas R.; Garge, Nikhil; Zhang, Xinxin; Sun, Wei; O'Connell, Thomas M.; Bunger, Maureen K.; Bultman, Scott J. (4 May 2011). "The Microbiome and Butyrate Regulate Energy Metabolism and Autophagy in the Mammalian Colon". Cell Metabolism 13 (5): 517–526. doi:10.1016/j.cmet.2011.02.018. ISSN 1550-4131. PMID 21531334.
- ↑ "triacylglycerol lipase – Homo sapiens". BRENDA. Technische Universität Braunschweig.. http://www.brenda-enzymes.org/enzyme.php?ecno=3.1.1.3&Suchword=&organism%5B%5D=Homo+sapiens&show_tm=0.
- ↑ "Microbiota and diabetes: an evolving relationship". Gut 63 (9): 1513–1521. September 2014. doi:10.1136/gutjnl-2014-306928. PMID 24833634.
- ↑ Cait, Alissa; Cardenas, Erick (December 2019). "Reduced genetic potential for butyrate fermentation in the gut microbiome of infants who develop allergic sensitization". Journal of Allergy and Clinical Immunology 144 (6): 1638–1647. E3. doi:10.1016/j.jaci.2019.06.029. PMID 31279007.
- ↑ Vatanen, T.Expression error: Unrecognized word "et". (2018). "The human gut microbiome in early-onset type 1 diabetes from the TEDDY study". Nature 562 (7728): 589–594. doi:10.1038/s41586-018-0620-2. PMID 30356183. Bibcode: 2018Natur.562..589V.
- ↑ "Molecular link between dietary fibre, gut microbiota and health". Molecular Biology Reports 47 (8): 6229–6237. 2020. doi:10.1007/s11033-020-05611-3. PMID 32623619.
- ↑ Consolandi, Clarissa; Turroni, Silvia; Emmi, Giacomo et al. (April 2015). "Behçet's syndrome patients exhibit specific microbiome signature". Autoimmunity Reviews 14 (4): 269–276. doi:10.1016/j.autrev.2014.11.009. PMID 25435420.
- ↑ Ye, Zi; Zhang, Ni; Wu, Chunyan et al. (4 August 2018). "A metagenomic study of the gut microbiome in Behcet's disease". Microbiome 6 (1): 135. doi:10.1186/s40168-018-0520-6. PMID 30077182.
- ↑ Cait, Alissa; Hughes, Michael R (May 2018). "Microbiome-driven allergic lung inflammation is ameliorated by short chain fatty acids". Mucosal Immunology 11 (3): 785–796. doi:10.1038/mi.2017.75. PMID 29067994.
- ↑ Furusawa, Yukihiro; Obata, Yuuki; Fukuda, Shinji et al. (13 November 2013). "Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells". Nature 504 (7480): 446–450. doi:10.1038/nature12721. PMID 24226770. Bibcode: 2013Natur.504..446F.
- ↑ Arpaia, Nicholas; Campbell, Clarissa; Fan, Xiying et al. (13 November 2013). "Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation". Nature 504 (7480): 451–455. doi:10.1038/nature12726. PMID 24226773. Bibcode: 2013Natur.504..451A.
- ↑ Luu, Maik; Weigand, Katharina; Wedi, Fatana et al. (26 September 2018). "Regulation of the effector function of CD8+ T cells by gut microbiota-derived metabolite butyrate". Scientific Reports 8 (1): 14430. doi:10.1038/s41598-018-32860-x. PMID 30258117. Bibcode: 2018NatSR...814430L.
- ↑ Cholan, Pradeep Manuneedhi; Han, Alvin; Woodie, Brad R.; Watchon, Maxinne; Kurz, Angela RM; Laird, Angela S.; Britton, Warwick J.; Ye, Lihua et al. (2020-11-09). "Conserved anti-inflammatory effects and sensing of butyrate in zebrafish". Gut Microbes 12 (1): 1–11. doi:10.1080/19490976.2020.1824563. ISSN 1949-0976. PMID 33064972.
- ↑ Vital, Marius; Gao, Jiarong; Rizzo, Mike; Harrison, Tara; Tiedje, James M. (2015). "Diet is a major factor governing the fecal butyrate-producing community structure across Mammalia, Aves and Reptilia". The ISME Journal 9 (4): 832–843. doi:10.1038/ismej.2014.179. PMID 25343515. Bibcode: 2015ISMEJ...9..832V.
- ↑ 57.0 57.1 57.2 57.3 "Human antimicrobial peptides and proteins". Pharmaceuticals 7 (5): 545–94. 2014. doi:10.3390/ph7050545. PMID 24828484.
Table 3: Select human antimicrobial peptides and their proposed targets
Table 4: Some known factors that induce antimicrobial peptide expression - ↑ "Destructive effects of butyrate on the cell envelope of Helicobacter pylori". J. Med. Microbiol. 61 (Pt 4): 582–9. 2012. doi:10.1099/jmm.0.039040-0. PMID 22194341.
- ↑ "Cholesterol enhances Helicobacter pylori resistance to antibiotics and LL-37". Antimicrob. Agents Chemother. 55 (6): 2897–904. 2011. doi:10.1128/AAC.00016-11. PMID 21464244.
- ↑ "Butyrate suppresses colonic inflammation through HDAC1-dependent Fas upregulation and Fas-mediated apoptosis of T cells". Am. J. Physiol. Gastrointest. Liver Physiol. 302 (12): G1405–15. 2012. doi:10.1152/ajpgi.00543.2011. PMID 22517765.
- ↑ "Nutritional or pharmacological activation of HCA(2) ameliorates neuroinflammation". Trends Mol Med 21 (4): 245–255. 2015. doi:10.1016/j.molmed.2015.02.002. PMID 25766751.
- ↑ "GPR109A and vascular inflammation". Curr Atheroscler Rep 15 (5): 325. May 2013. doi:10.1007/s11883-013-0325-9. PMID 23526298.
- ↑ "Anti-inflammatory effects of the hydroxycarboxylic acid receptor 2". Metab. Clin. Exp. 65 (2): 102–113. February 2016. doi:10.1016/j.metabol.2015.10.001. PMID 26773933.
- ↑ "The homeostatic role of neuropeptide Y in immune function and its impact on mood and behaviour". Acta Physiol (Oxf) 213 (3): 603–27. 2015. doi:10.1111/apha.12445. PMID 25545642.
- ↑ Zeng, Huawei; Lazarova, DL; Bordonaro, M (2014). "Mechanisms linking dietary fiber, gut microbiota and colon cancer prevention". World Journal of Gastrointestinal Oncology 6 (2): 41–51. doi:10.4251/wjgo.v6.i2.41. PMID 24567795.
- ↑ Chen, Jiezhong; Zhao, Kong-Nan; Vitetta, Luis (2019). "Effects of Intestinal Microbial–Elaborated Butyrate on Oncogenic Signaling Pathways" (pdf). Nutrients 11 (5): 1026. doi:10.3390/nu11051026. PMID 31067776. PMC 6566851. https://www.mdpi.com/2072-6643/11/5/1026/pdf.
- ↑ "Oncogenic Ras promotes butyrate-induced apoptosis through inhibition of gelsolin expression". The Journal of Biological Chemistry 279 (35): 36680–8. August 2004. doi:10.1074/jbc.M405197200. PMID 15213223.
- ↑ Bereswill, Stefan, ed (2009). "Butyrate-induced transcriptional changes in human colonic mucosa". PLOS ONE 4 (8): e6759. doi:10.1371/journal.pone.0006759. PMID 19707587. Bibcode: 2009PLoSO...4.6759V.
- ↑ Encarnação, J. C.; Abrantes, A. M.; Pires, A. S. et al. (30 July 2015). "Revisit dietary fiber on colorectal cancer: butyrate and its role on prevention and treatment". Cancer and Metastasis Reviews 34 (3): 465–478. doi:10.1007/s10555-015-9578-9. PMID 26224132.
- ↑ Zimmerman, Mary A.; Singh, Nagendra; Martin, Pamela M. et al. (15 June 2012). "Butyrate suppresses colonic inflammation through HDAC1-dependent Fas upregulation and Fas-mediated apoptosis of T cells". American Journal of Physiology. Gastrointestinal and Liver Physiology 302 (12): G1405–G1415. doi:10.1152/ajpgi.00543.2011. PMID 22517765.
- ↑ Prasanna Kumar, S.; Thippeswamy, G.; Sheela, M.L. et al. (October 2008). "Butyrate-induced phosphatase regulates VEGF and angiogenesis via Sp1". Archives of Biochemistry and Biophysics 478 (1): 85–95. doi:10.1016/j.abb.2008.07.004. PMID 18655767.
- ↑ "Low-carb diet cuts risk of colon cancer, study finds | University of Toronto Media Room". https://media.utoronto.ca/media-releases/low-carb-diet-cuts-risk-of-colon-cancer-study-finds/.
- ↑ Belcheva, Antoaneta; Irrazabal, Thergiory; Robertson, Susan J.; Streutker, Catherine; Maughan, Heather; Rubino, Stephen; Moriyama, Eduardo H.; Copeland, Julia K. et al. (2014-07-17). "Gut microbial metabolism drives transformation of MSH2-deficient colon epithelial cells". Cell 158 (2): 288–299. doi:10.1016/j.cell.2014.04.051. ISSN 1097-4172. PMID 25036629.
- ↑ Scheppach, W.; Sommer, H.; Kirchner, T. et al. (1992). "Effect of butyrate enemas on the colonic mucosa in distal ulcerative colitis". Gastroenterology 103 (1): 51–56. doi:10.1016/0016-5085(92)91094-K. PMID 1612357.
- ↑ "Transcriptional and epigenetic mechanisms of addiction". Nat. Rev. Neurosci. 12 (11): 623–637. November 2011. doi:10.1038/nrn3111. PMID 21989194.
- ↑ "Epigenetic mechanisms of drug addiction". Neuropharmacology 76 Pt B: 259–268. January 2014. doi:10.1016/j.neuropharm.2013.04.004. PMID 23643695.
- ↑ 77.0 77.1 "Regulation of chromatin states by drugs of abuse". Curr. Opin. Neurobiol. 30: 112–121. February 2015. doi:10.1016/j.conb.2014.11.002. PMID 25486626.
- ↑ "Epigenetics: a link between addiction and social environment". Cellular and Molecular Life Sciences 74 (15): 2735–2747. August 2017. doi:10.1007/s00018-017-2493-1. PMID 28255755.
- ↑ "Mécanismes épigénétiques et troubles de l'usage d'alcool : une cible thérapeutique intéressante?" (in fr). Biologie Aujourd'hui 211 (1): 83–91. 2017. doi:10.1051/jbio/2017014. PMID 28682229.
External links
 |